Conditionally Active Immuno-oncology Therapeutics October 2025 .2
Disclaimer This presentation has been prepared by Sensei Biotherapeutics, Inc. (the “Company,” "we," "us") and is made for informational purposes only. The information set forth herein does not purport to be complete or to contain all of the information you may desire. Statements contained herein are made as of the date of this presentation unless stated otherwise, and the delivery of this presentation at any time shall not under any circumstances create an implication that the information contained herein is correct as of any time after such date or that information will be updated or revised to reflect information that subsequently becomes available or changes occurring after the date hereof. This presentation contains estimates and other statistical data made by independent parties and by us relating to market shares and other data about our industry. This presentation also contains "forward-looking" statements as that term is defined in the Private Securities Litigation Reform Act of 1995 that are based on our management's beliefs and assumptions and on information currently available to management. These forward-looking statements include, without limitation, expectations regarding the development and potential therapeutic benefits of our product candidates; the expected safety, pharmacokinetic and efficacy profile of our product candidates, including Solnerstotug; the expected timing of clinical data from our Phase 1/2 clinical trial of Solnerstotug and the expansion of the Phase 1 clinical trial to include additional patients with specific tumor types. When used in this presentation, the words and phrases "designed to," "may," "believes," "intends," "seeks," "anticipates," "plans," "estimates," "expects," "should," "assumes," "continues," "could," "will," "future" and the negative of these or similar terms and phrases are intended to identify forward-looking statements. Forward-looking statements involve known and unknown risks, uncertainties and other factors that may cause our actual results, performance or achievements to be materially different from any future results, performance or achievements expressed or implied by the forward-looking statements. Risks and uncertainties that may cause actual results to differ materially include uncertainties inherent in the development of therapeutic product candidates, such as preclinical discovery and development; conduct of clinical trials and related regulatory requirements, including the risk of delay or cessation of any clinical trials of Sensei’s product candidates; the risk that prior results, such as signals of safety, activity or durability of effect, observed from preclinical trials and early results from the clinical trial of Solnerstotug, will not be replicated or will not continue in ongoing or future studies or clinical trials involving Sensei’s product candidates, including Solnerstotug; our reliance on third parties over which we may not always have full control; risks regarding the accuracy of our estimates of expenses, capital requirements and needs for additional financing; and other risk and uncertainties that are described in our Quarterly Report on Form 10-Q filed with the SEC on August 5, 2025 and our other Periodic Reports filed with the SEC. Forward-looking statements represent our management's beliefs and assumptions only as of the date of this presentation and include all matters that are not historical facts. Our actual future results may be materially different from what we expect. Except as required by law, we assume no obligation to update these forward-looking statements publicly, or to update the reasons actual results could differ materially from those anticipated in the forward-looking statements, even if new information becomes available in the future. Certain information contained in this presentation relates to, or is based on, studies, publications, surveys and other data obtained from third-party sources and the Company's own internal estimates and research. While the Company believes these third-party sources to be reliable as of the date of this presentation, it has not independently verified, and makes no representation as to the adequacy, fairness, accuracy or completeness of, any information obtained from third-party sources. In addition, all of the market data included in this presentation involves a number of assumptions and limitations, and there can be no guarantee as to the accuracy or reliability of such assumptions. Finally, while we believe our own internal research is reliable, such research has not been verified by any independent source.
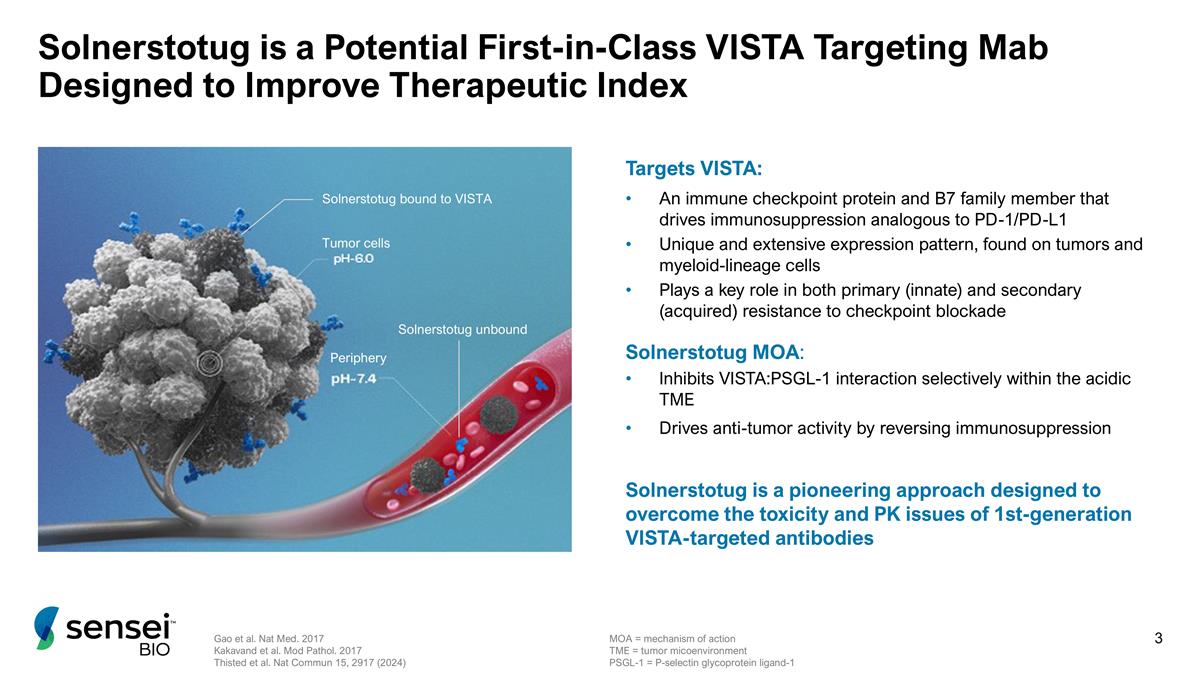
Solnerstotug is a Potential First-in-Class VISTA Targeting Mab Designed to Improve Therapeutic Index Tumor cells Periphery Solnerstotug bound to VISTA Solnerstotug unbound Targets VISTA: An immune checkpoint protein and B7 family member that drives immunosuppression analogous to PD-1/PD-L1 Unique and extensive expression pattern, found on tumors and myeloid-lineage cells Plays a key role in both primary (innate) and secondary (acquired) resistance to checkpoint blockade Solnerstotug MOA: Inhibits VISTA:PSGL-1 interaction selectively within the acidic TME Drives anti-tumor activity by reversing immunosuppression Solnerstotug is a pioneering approach designed to overcome the toxicity and PK issues of 1st-generation VISTA-targeted antibodies Gao et al. Nat Med. 2017 Kakavand et al. Mod Pathol. 2017 Thisted et al. Nat Commun 15, 2917 (2024) MOA = mechanism of action TME = tumor micoenvironment PSGL-1 = P-selectin glycoprotein ligand-1
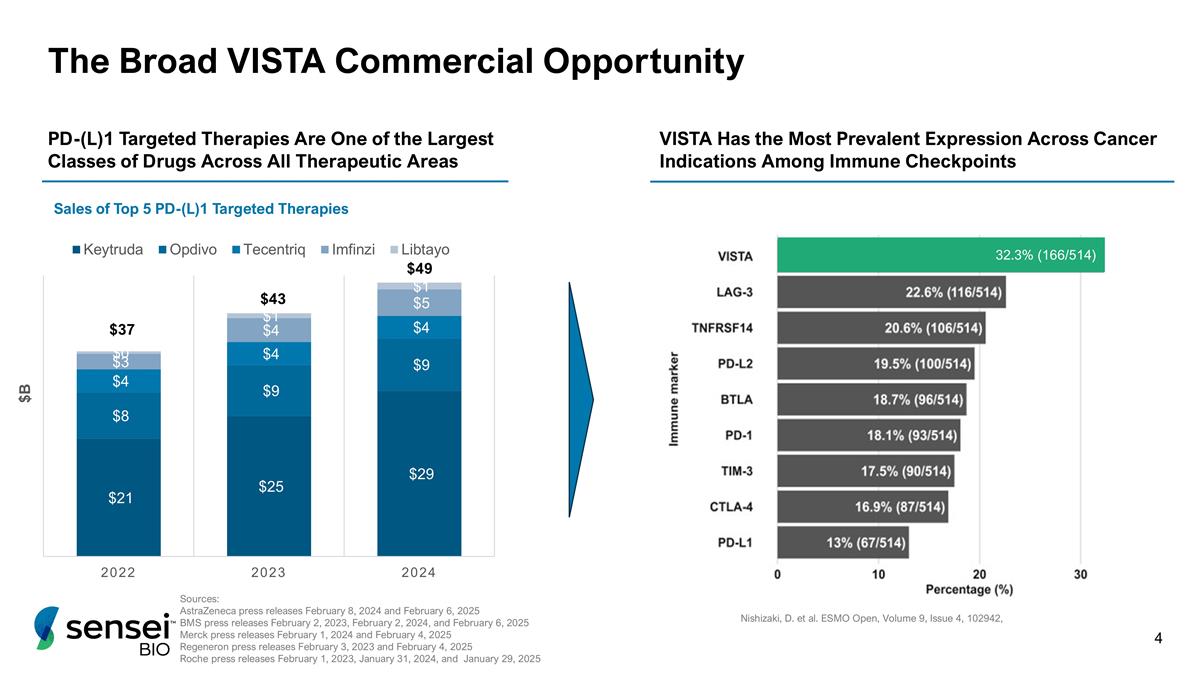
The Broad VISTA Commercial Opportunity Nishizaki, D. et al. ESMO Open, Volume 9, Issue 4, 102942, VISTA Has the Most Prevalent Expression Across Cancer Indications Among Immune Checkpoints 32.3% (166/514) Sources: AstraZeneca press releases February 8, 2024 and February 6, 2025 BMS press releases February 2, 2023, February 2, 2024, and February 6, 2025 Merck press releases February 1, 2024 and February 4, 2025 Regeneron press releases February 3, 2023 and February 4, 2025 Roche press releases February 1, 2023, January 31, 2024, and January 29, 2025 Sales of Top 5 PD-(L)1 Targeted Therapies PD-(L)1 Targeted Therapies Are One of the Largest Classes of Drugs Across All Therapeutic Areas $37 $43 $49
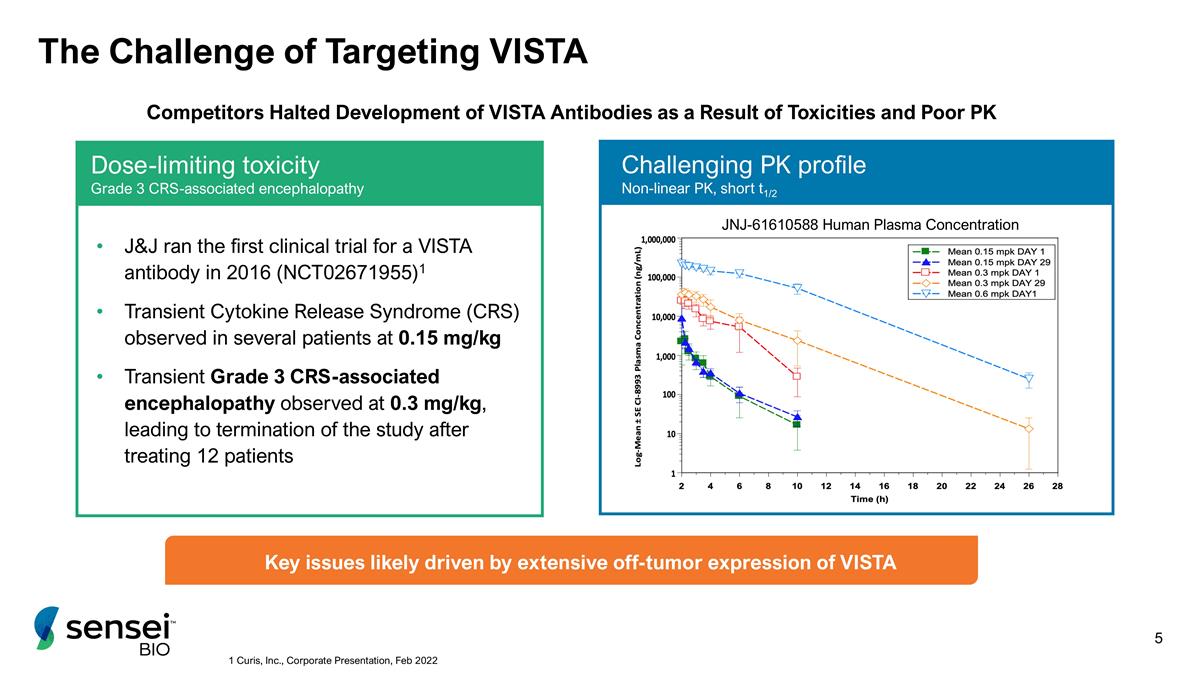
Dose-limiting toxicity Grade 3 CRS-associated encephalopathy The Challenge of Targeting VISTA JNJ-61610588 Human Plasma Concentration J&J ran the first clinical trial for a VISTA antibody in 2016 (NCT02671955)1 Transient Cytokine Release Syndrome (CRS) observed in several patients at 0.15 mg/kg Transient Grade 3 CRS-associated encephalopathy observed at 0.3 mg/kg, leading to termination of the study after treating 12 patients Challenging PK profile Non-linear PK, short t1/2 1 Curis, Inc., Corporate Presentation, Feb 2022 Competitors Halted Development of VISTA Antibodies as a Result of Toxicities and Poor PK Key issues likely driven by extensive off-tumor expression of VISTA
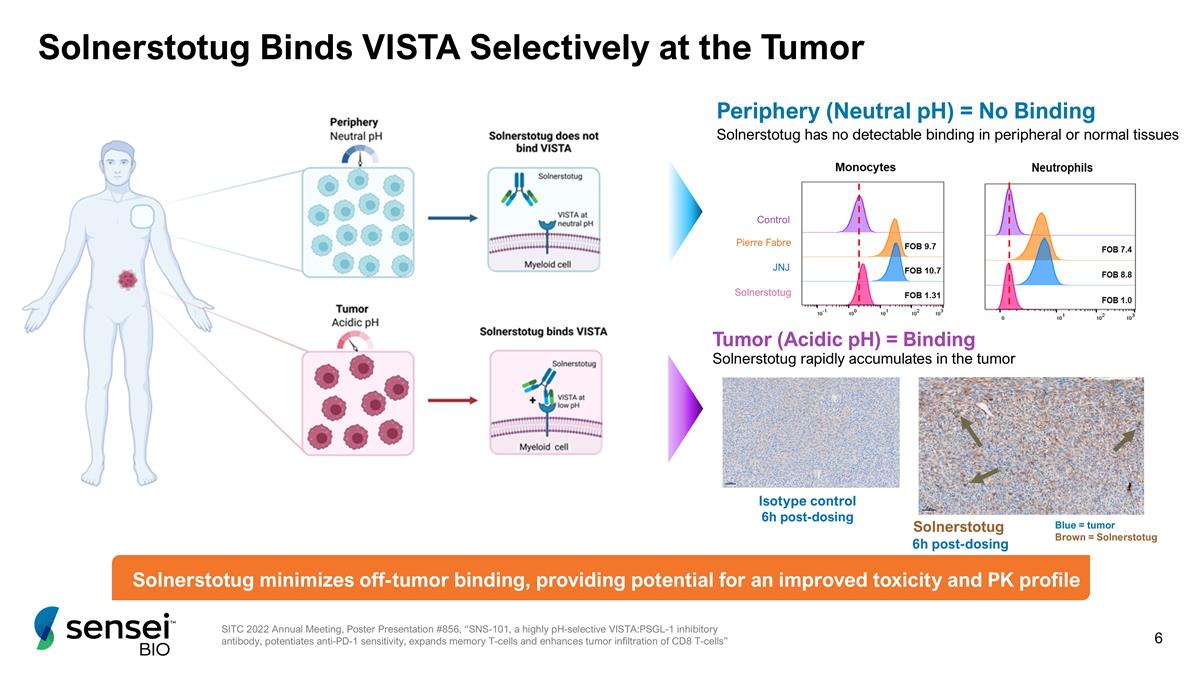
Solnerstotug Binds VISTA Selectively at the Tumor Pierre Fabre JNJ Solnerstotug Control Periphery (Neutral pH) = No Binding Solnerstotug has no detectable binding in peripheral or normal tissues Solnerstotug rapidly accumulates in the tumor Solnerstotug 6h post-dosing Isotype control 6h post-dosing Blue = tumor Brown = Solnerstotug Tumor (Acidic pH) = Binding Solnerstotug minimizes off-tumor binding, providing potential for an improved toxicity and PK profile SITC 2022 Annual Meeting, Poster Presentation #856, “SNS-101, a highly pH-selective VISTA:PSGL-1 inhibitory antibody, potentiates anti-PD-1 sensitivity, expands memory T-cells and enhances tumor infiltration of CD8 T-cells”
Solnerstotug Dose Escalation Data
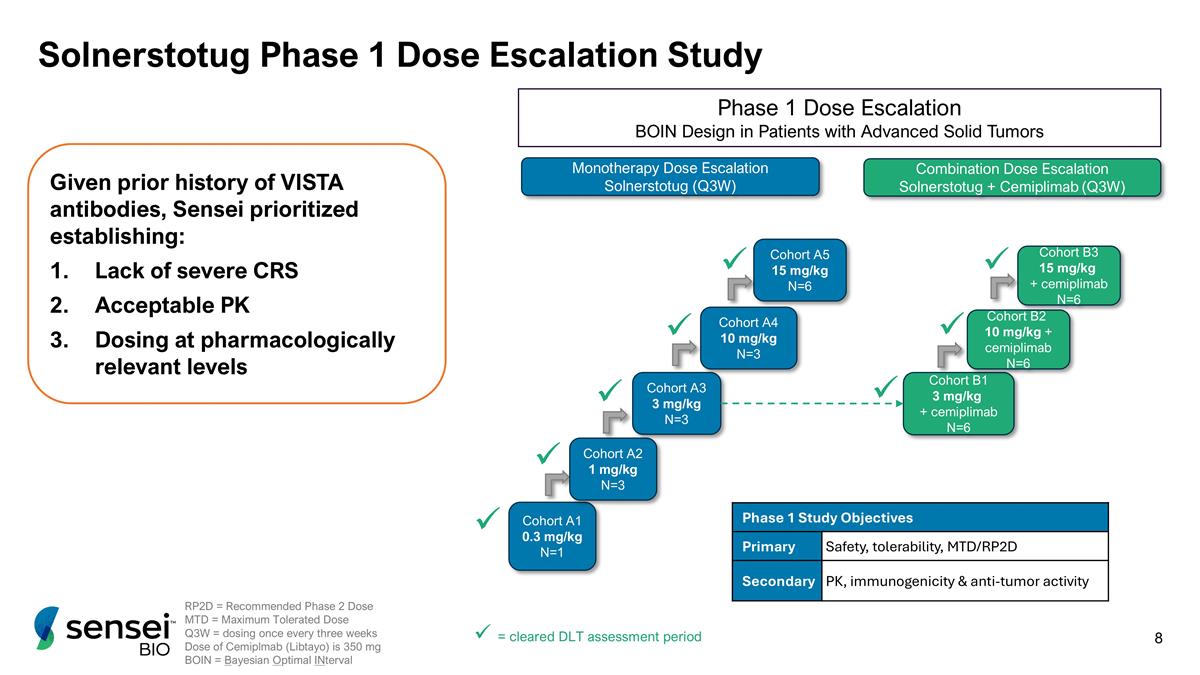
Solnerstotug Phase 1 Dose Escalation Study Cohort A1 0.3 mg/kg N=1 Cohort B1 3 mg/kg + cemiplimab N=6 Cohort A2 1 mg/kg N=3 Cohort A3 3 mg/kg N=3 Cohort A4 10 mg/kg N=3 Cohort A5 15 mg/kg N=6 Cohort B2 10 mg/kg + cemiplimab N=6 Cohort B3 15 mg/kg + cemiplimab N=6 Monotherapy Dose Escalation Solnerstotug (Q3W) Combination Dose Escalation Solnerstotug + Cemiplimab (Q3W) Phase 1 Dose Escalation BOIN Design in Patients with Advanced Solid Tumors ü ü ü ü Phase 1 Study Objectives Primary Safety, tolerability, MTD/RP2D Secondary PK, immunogenicity & anti-tumor activity RP2D = Recommended Phase 2 Dose MTD = Maximum Tolerated Dose Q3W = dosing once every three weeks Dose of Cemiplmab (Libtayo) is 350 mg BOIN = Bayesian Optimal INterval ü ü ü = cleared DLT assessment period ü ü Given prior history of VISTA antibodies, Sensei prioritized establishing: Lack of severe CRS Acceptable PK Dosing at pharmacologically relevant levels
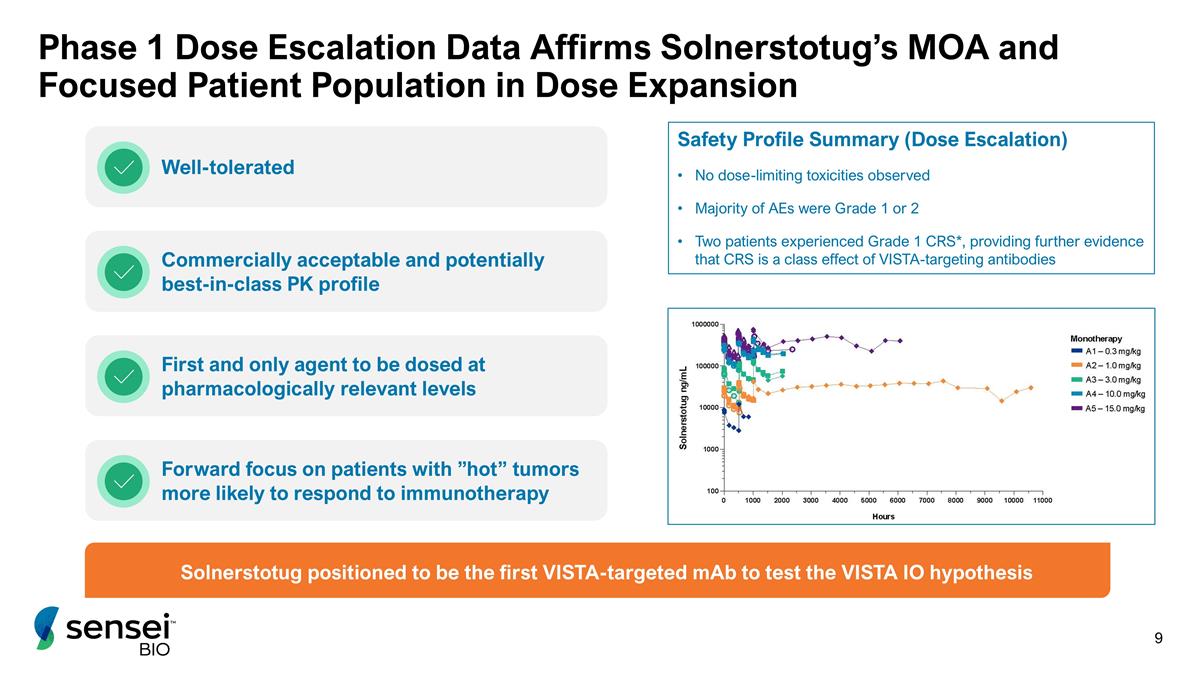
Phase 1 Dose Escalation Data Affirms Solnerstotug’s MOA and Focused Patient Population in Dose Expansion Solnerstotug positioned to be the first VISTA-targeted mAb to test the VISTA IO hypothesis Well-tolerated Commercially acceptable and potentially best-in-class PK profile First and only agent to be dosed at pharmacologically relevant levels Forward focus on patients with ”hot” tumors more likely to respond to immunotherapy Safety Profile Summary (Dose Escalation) No dose-limiting toxicities observed Majority of AEs were Grade 1 or 2 Two patients experienced Grade 1 CRS*, providing further evidence that CRS is a class effect of VISTA-targeting antibodies
Solnerstotug Dose Expansion Data
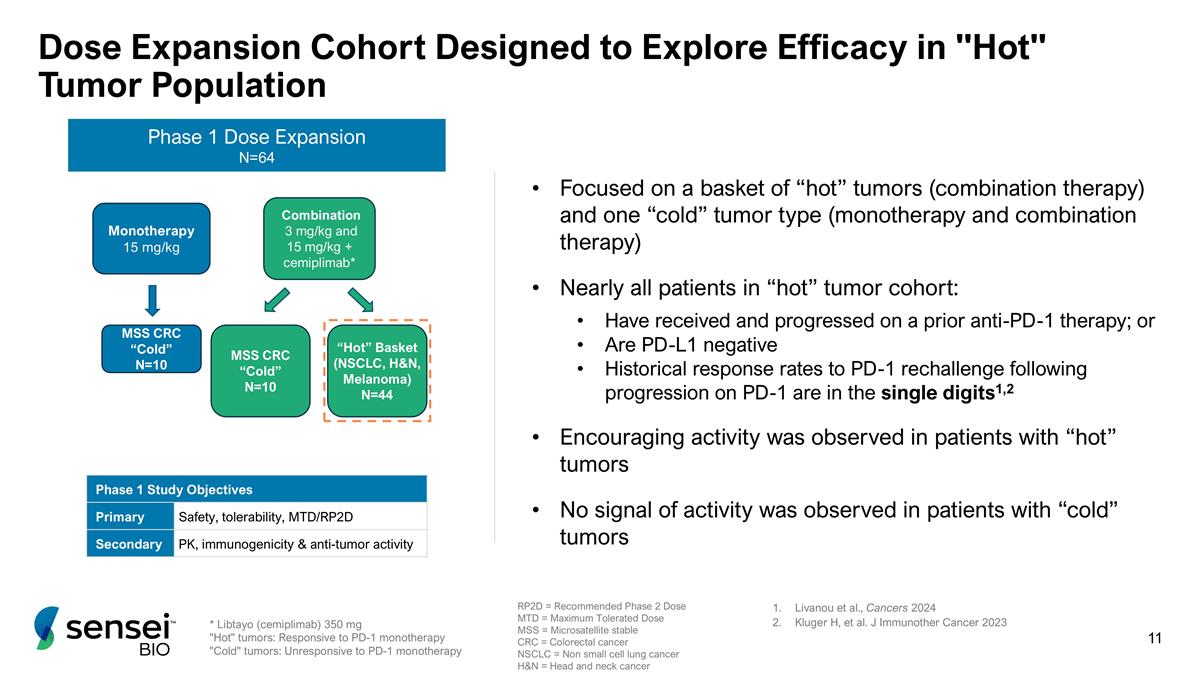
Dose Expansion Cohort Designed to Explore Efficacy in "Hot" Tumor Population * Libtayo (cemiplimab) 350 mg "Hot" tumors: Responsive to PD-1 monotherapy "Cold" tumors: Unresponsive to PD-1 monotherapy MSS CRC “Cold” N=10 MSS CRC “Cold” N=10 Phase 1 Dose Expansion N=64 Phase 1 Study Objectives Primary Safety, tolerability, MTD/RP2D Secondary PK, immunogenicity & anti-tumor activity RP2D = Recommended Phase 2 Dose MTD = Maximum Tolerated Dose MSS = Microsatellite stable CRC = Colorectal cancer NSCLC = Non small cell lung cancer H&N = Head and neck cancer Monotherapy 15 mg/kg Combination 3 mg/kg and 15 mg/kg + cemiplimab* Focused on a basket of “hot” tumors (combination therapy) and one “cold” tumor type (monotherapy and combination therapy) Nearly all patients in “hot” tumor cohort: Have received and progressed on a prior anti-PD-1 therapy; or Are PD-L1 negative Historical response rates to PD-1 rechallenge following progression on PD-1 are in the single digits1,2 Encouraging activity was observed in patients with “hot” tumors No signal of activity was observed in patients with “cold” tumors Livanou et al., Cancers 2024 Kluger H, et al. J Immunother Cancer 2023 “Hot” Basket (NSCLC, H&N, Melanoma) N=44
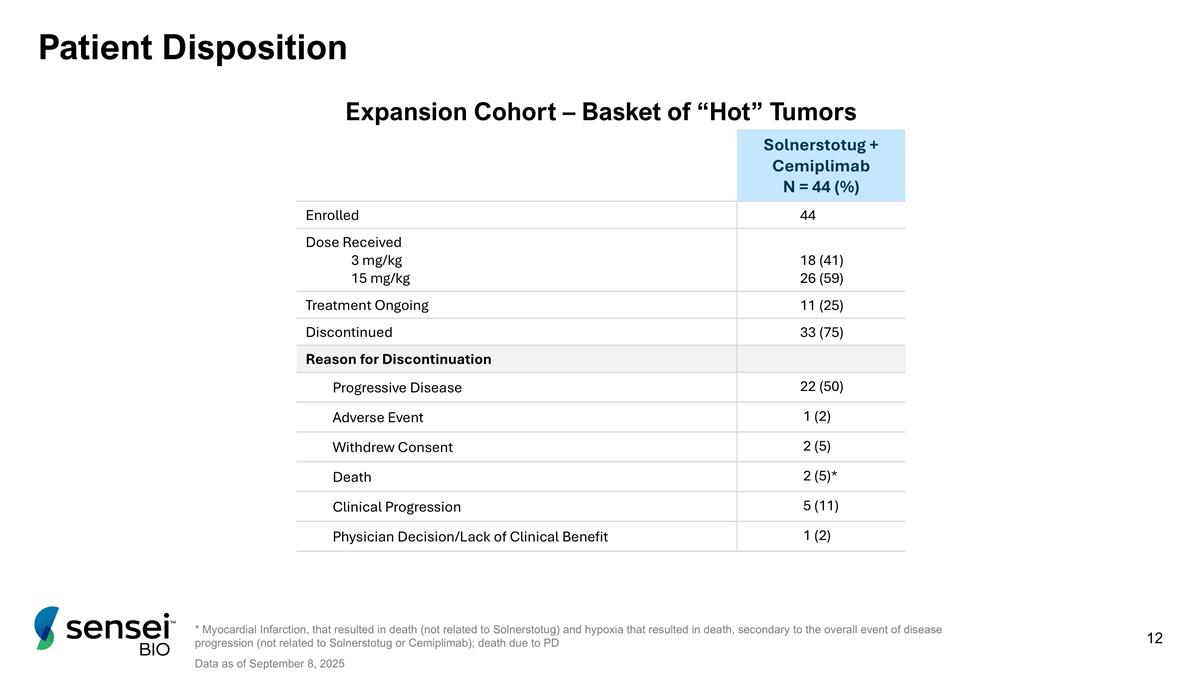
Patient Disposition Solnerstotug + Cemiplimab N = 44 (%) Enrolled 44 Dose Received 3 mg/kg 15 mg/kg 18 (41) 26 (59) Treatment Ongoing 11 (25) Discontinued 33 (75) Reason for Discontinuation Progressive Disease 22 (50) Adverse Event 1 (2) Withdrew Consent 2 (5) Death 2 (5)* Clinical Progression 5 (11) Physician Decision/Lack of Clinical Benefit 1 (2) * Myocardial Infarction, that resulted in death (not related to Solnerstotug) and hypoxia that resulted in death, secondary to the overall event of disease progression (not related to Solnerstotug or Cemiplimab); death due to PD Data as of September 8, 2025 Expansion Cohort – Basket of “Hot” Tumors
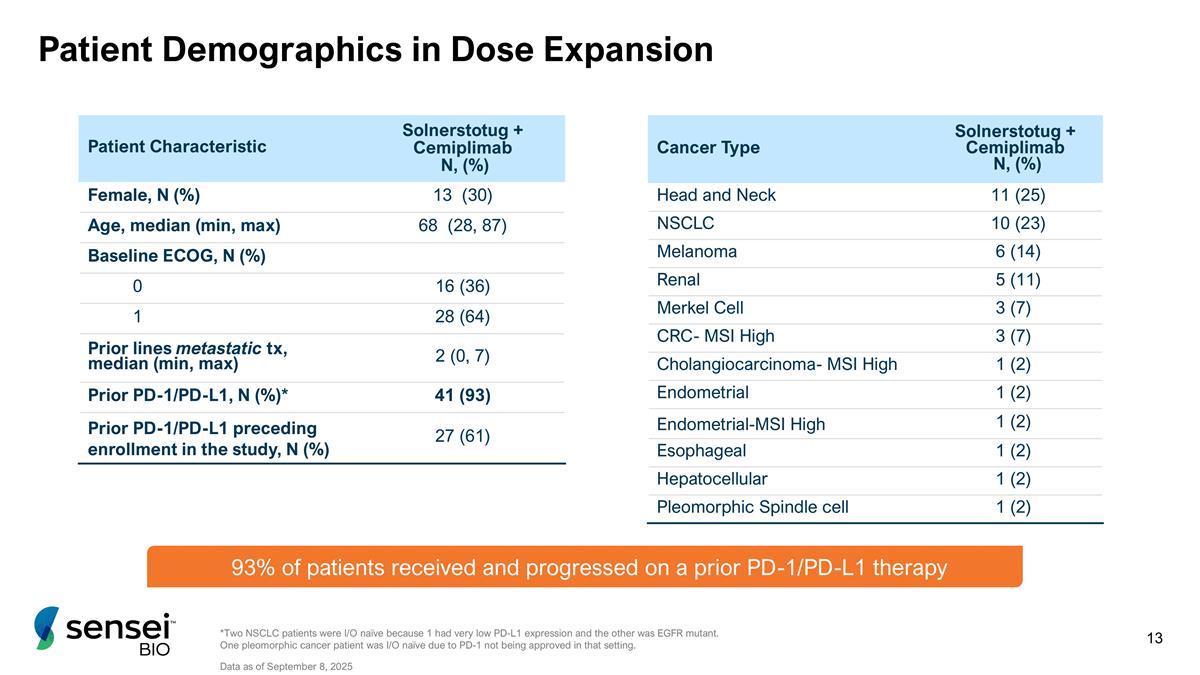
Patient Demographics in Dose Expansion Patient Characteristic Solnerstotug + Cemiplimab N, (%) Female, N (%) 13 (30) Age, median (min, max) 68 (28, 87) Baseline ECOG, N (%) 0 16 (36) 1 28 (64) Prior lines metastatic tx, median (min, max) 2 (0, 7) Prior PD-1/PD-L1, N (%)* 41 (93) Prior PD-1/PD-L1 preceding enrollment in the study, N (%) 27 (61) Cancer Type Solnerstotug + Cemiplimab N, (%) Head and Neck 11 (25) NSCLC 10 (23) Melanoma 6 (14) Renal 5 (11) Merkel Cell 3 (7) CRC- MSI High 3 (7) Cholangiocarcinoma- MSI High 1 (2) Endometrial 1 (2) Endometrial-MSI High 1 (2) Esophageal 1 (2) Hepatocellular 1 (2) Pleomorphic Spindle cell 1 (2) *Two NSCLC patients were I/O naïve because 1 had very low PD-L1 expression and the other was EGFR mutant. One pleomorphic cancer patient was I/O naïve due to PD-1 not being approved in that setting. Data as of September 8, 2025 93% of patients received and progressed on a prior PD-1/PD-L1 therapy
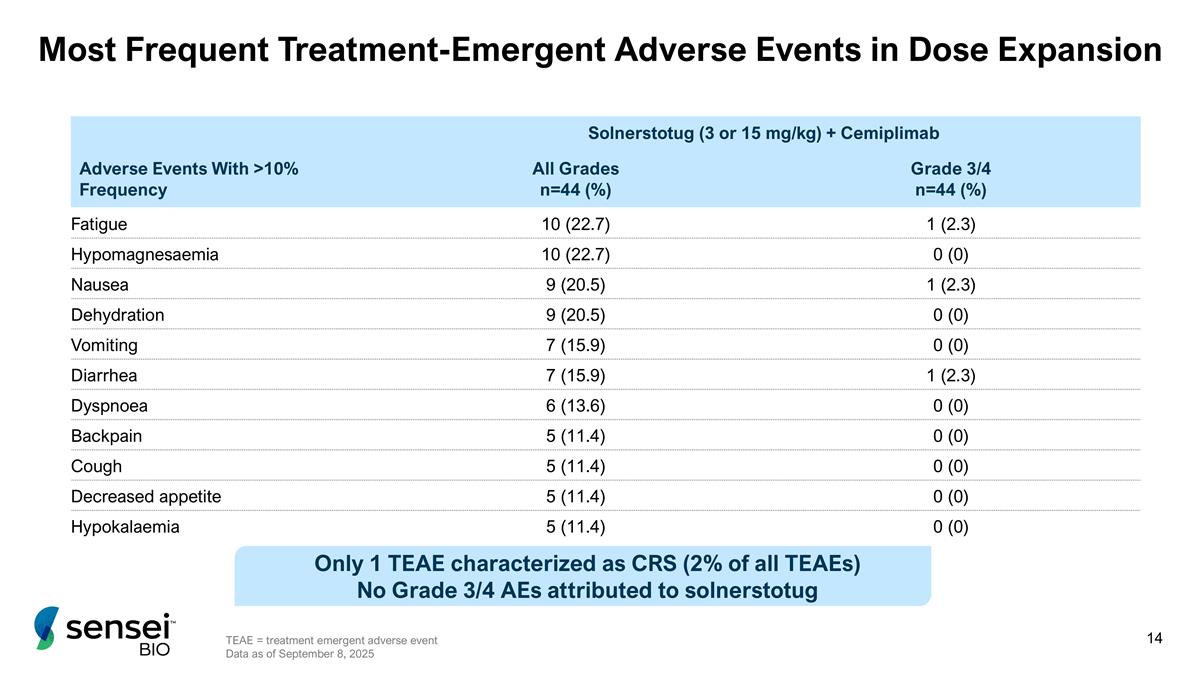
Most Frequent Treatment-Emergent Adverse Events in Dose Expansion Solnerstotug (3 or 15 mg/kg) + Cemiplimab Adverse Events With >10% Frequency All Grades n=44 (%) Grade 3/4 n=44 (%) Fatigue 10 (22.7) 1 (2.3) Hypomagnesaemia 10 (22.7) 0 (0) Nausea 9 (20.5) 1 (2.3) Dehydration 9 (20.5) 0 (0) Vomiting 7 (15.9) 0 (0) Diarrhea 7 (15.9) 1 (2.3) Dyspnoea 6 (13.6) 0 (0) Backpain 5 (11.4) 0 (0) Cough 5 (11.4) 0 (0) Decreased appetite 5 (11.4) 0 (0) Hypokalaemia 5 (11.4) 0 (0) Only 1 TEAE characterized as CRS (2% of all TEAEs) No Grade 3/4 AEs attributed to solnerstotug TEAE = treatment emergent adverse event Data as of September 8, 2025
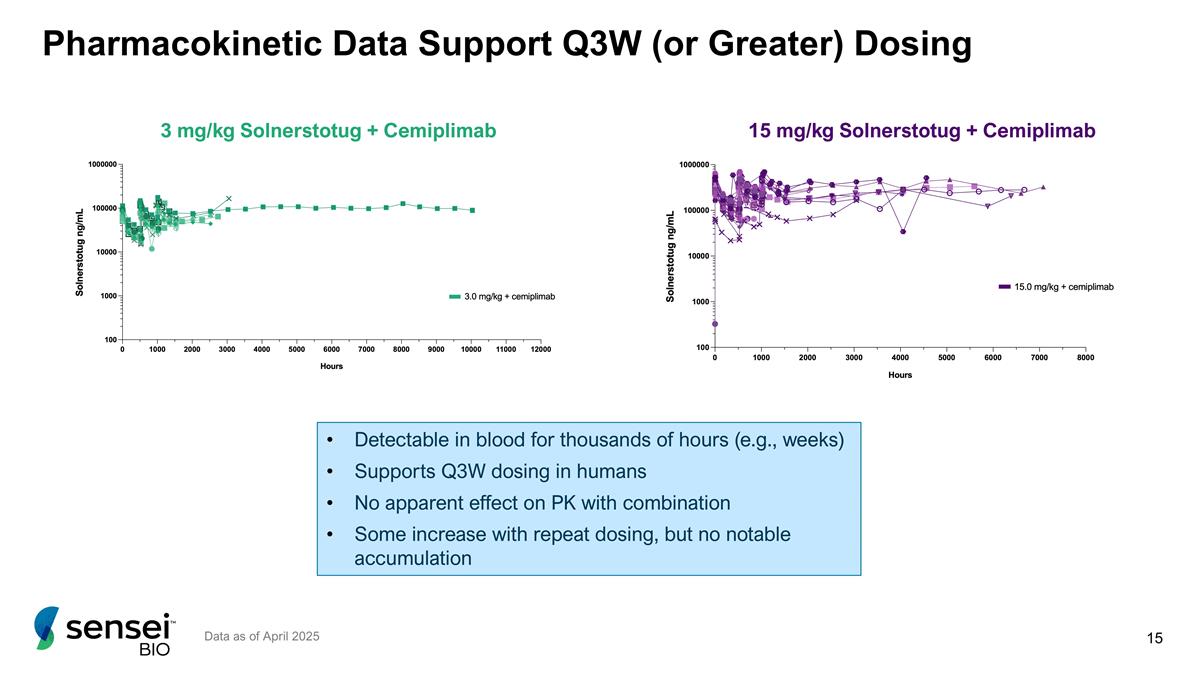
Pharmacokinetic Data Support Q3W (or Greater) Dosing Detectable in blood for thousands of hours (e.g., weeks) Supports Q3W dosing in humans No apparent effect on PK with combination Some increase with repeat dosing, but no notable accumulation Data as of April 2025 15 mg/kg Solnerstotug + Cemiplimab 3 mg/kg Solnerstotug + Cemiplimab
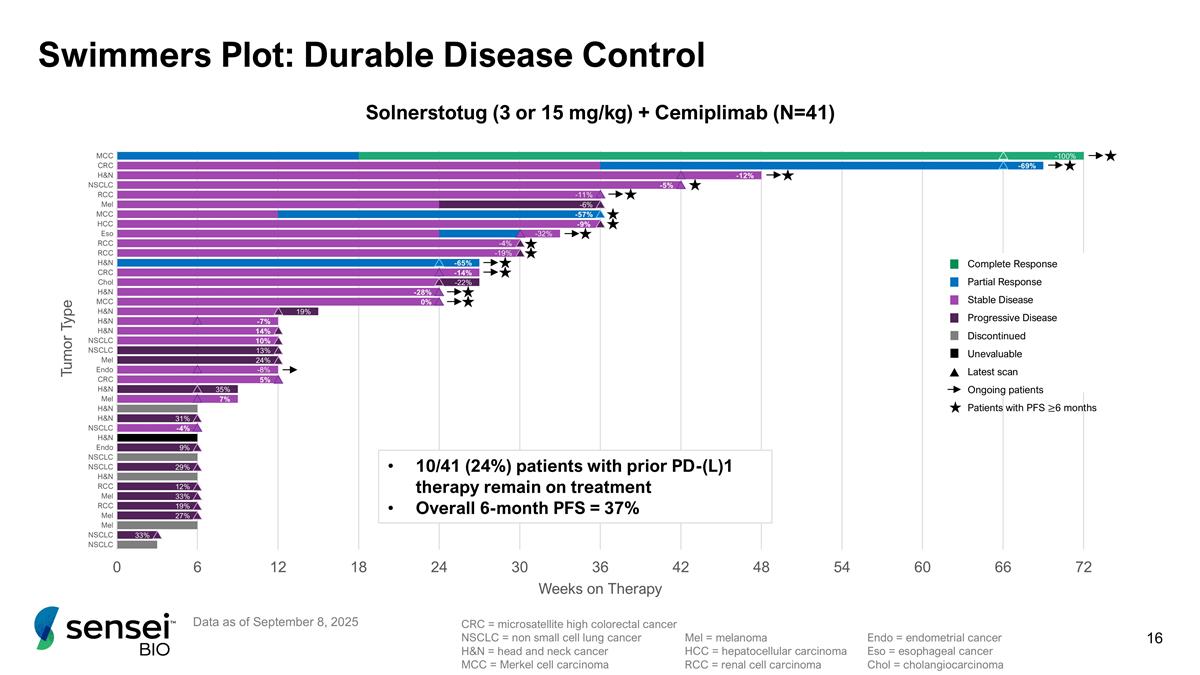
Swimmers Plot: Durable Disease Control Data as of September 8, 2025 10/41 (24%) patients with prior PD-(L)1 therapy remain on treatment Overall 6-month PFS = 37% CRC = microsatellite high colorectal cancer NSCLC = non small cell lung cancer H&N = head and neck cancer MCC = Merkel cell carcinoma Mel = melanoma HCC = hepatocellular carcinoma RCC = renal cell carcinoma Endo = endometrial cancer Eso = esophageal cancer Chol = cholangiocarcinoma Solnerstotug (3 or 15 mg/kg) + Cemiplimab (N=41) Complete Response Partial Response Stable Disease Progressive Disease Discontinued Unevaluable Latest scan Ongoing patients Patients with PFS ≥6 months
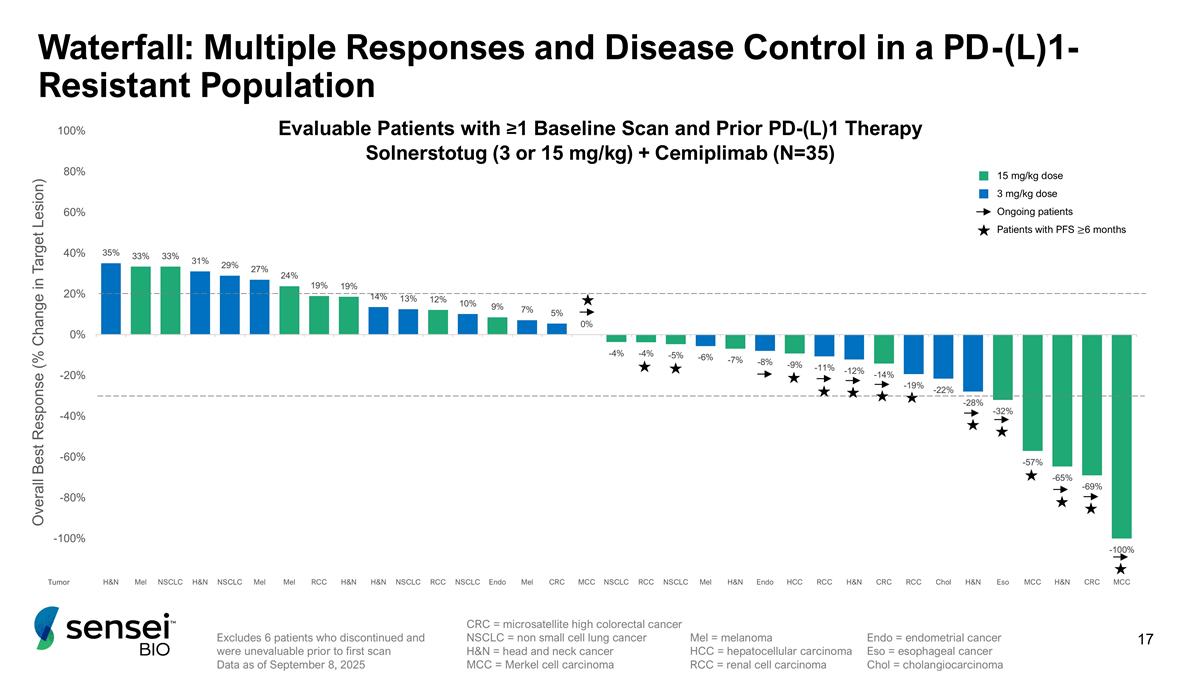
Excludes 6 patients who discontinued and were unevaluable prior to first scan Data as of September 8, 2025 Waterfall: Multiple Responses and Disease Control in a PD-(L)1-Resistant Population CRC = microsatellite high colorectal cancer NSCLC = non small cell lung cancer H&N = head and neck cancer MCC = Merkel cell carcinoma Mel = melanoma HCC = hepatocellular carcinoma RCC = renal cell carcinoma Endo = endometrial cancer Eso = esophageal cancer Chol = cholangiocarcinoma 15 mg/kg dose 3 mg/kg dose Ongoing patients Patients with PFS ≥6 months Evaluable Patients with ≥1 Baseline Scan and Prior PD-(L)1 Therapy Solnerstotug (3 or 15 mg/kg) + Cemiplimab (N=35)
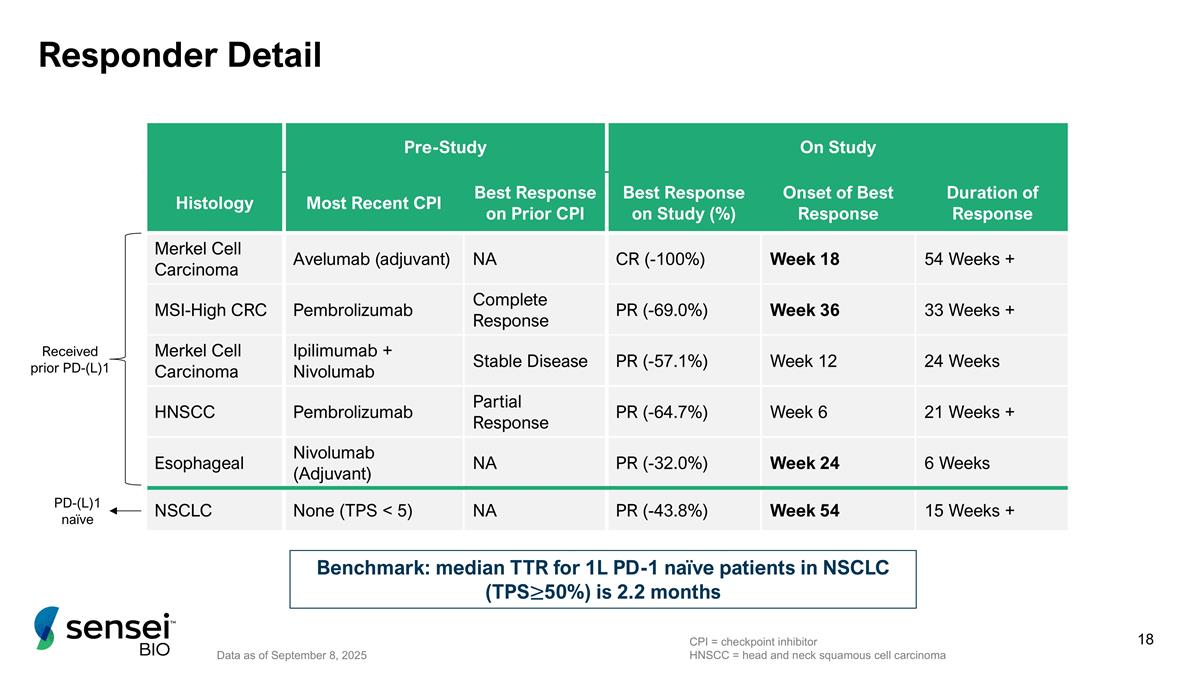
Responder Detail Data as of September 8, 2025 Pre-Study On Study Histology Most Recent CPI Best Response on Prior CPI Best Response on Study (%) Onset of Best Response Duration of Response Merkel Cell Carcinoma Avelumab (adjuvant) NA CR (-100%) Week 18 54 Weeks + MSI-High CRC Pembrolizumab Complete Response PR (-69.0%) Week 36 33 Weeks + Merkel Cell Carcinoma Ipilimumab + Nivolumab Stable Disease PR (-57.1%) Week 12 24 Weeks HNSCC Pembrolizumab Partial Response PR (-64.7%) Week 6 21 Weeks + Esophageal Nivolumab (Adjuvant) NA PR (-32.0%) Week 24 6 Weeks NSCLC None (TPS < 5) NA PR (-43.8%) Week 54 15 Weeks + Benchmark: median TTR for 1L PD-1 naïve patients in NSCLC (TPS≥50%) is 2.2 months CPI = checkpoint inhibitor HNSCC = head and neck squamous cell carcinoma Received prior PD-(L)1 PD-(L)1 naïve
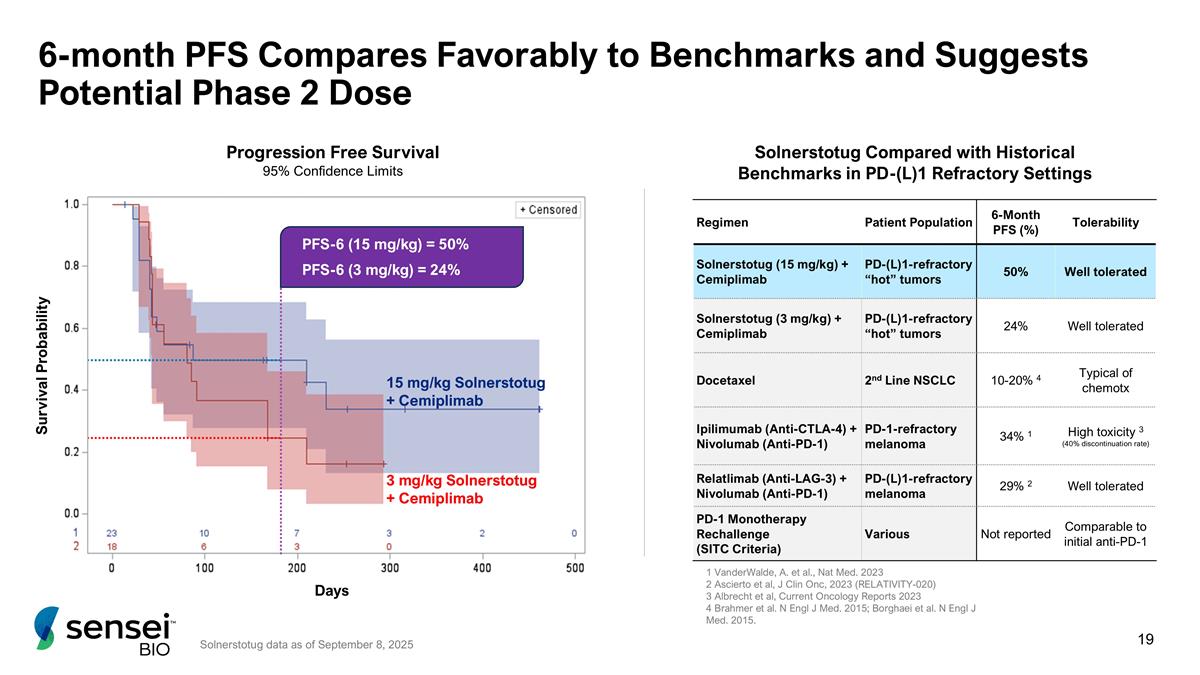
6-month PFS Compares Favorably to Benchmarks and Suggests Potential Phase 2 Dose 15 mg/kg Solnerstotug + Cemiplimab 3 mg/kg Solnerstotug + Cemiplimab PFS-6 (15 mg/kg) = 50% PFS-6 (3 mg/kg) = 24% Regimen Patient Population 6-Month PFS (%) Tolerability Solnerstotug (15 mg/kg) + Cemiplimab PD-(L)1-refractory “hot” tumors 50% Well tolerated Solnerstotug (3 mg/kg) + Cemiplimab PD-(L)1-refractory “hot” tumors 24% Well tolerated Docetaxel 2nd Line NSCLC 10-20% 4 Typical of chemotx Ipilimumab (Anti-CTLA-4) + Nivolumab (Anti-PD-1) PD-1-refractory melanoma 34% 1 High toxicity 3 (40% discontinuation rate) Relatlimab (Anti-LAG-3) + Nivolumab (Anti-PD-1) PD-(L)1-refractory melanoma 29% 2 Well tolerated PD-1 Monotherapy Rechallenge (SITC Criteria) Various Not reported Comparable to initial anti-PD-1 Progression Free Survival 95% Confidence Limits Days Survival Probability Solnerstotug Compared with Historical Benchmarks in PD-(L)1 Refractory Settings 1 VanderWalde, A. et al., Nat Med. 2023 2 Ascierto et al, J Clin Onc, 2023 (RELATIVITY-020) 3 Albrecht et al, Current Oncology Reports 2023 4 Brahmer et al. N Engl J Med. 2015; Borghaei et al. N Engl J Med. 2015. Solnerstotug data as of September 8, 2025
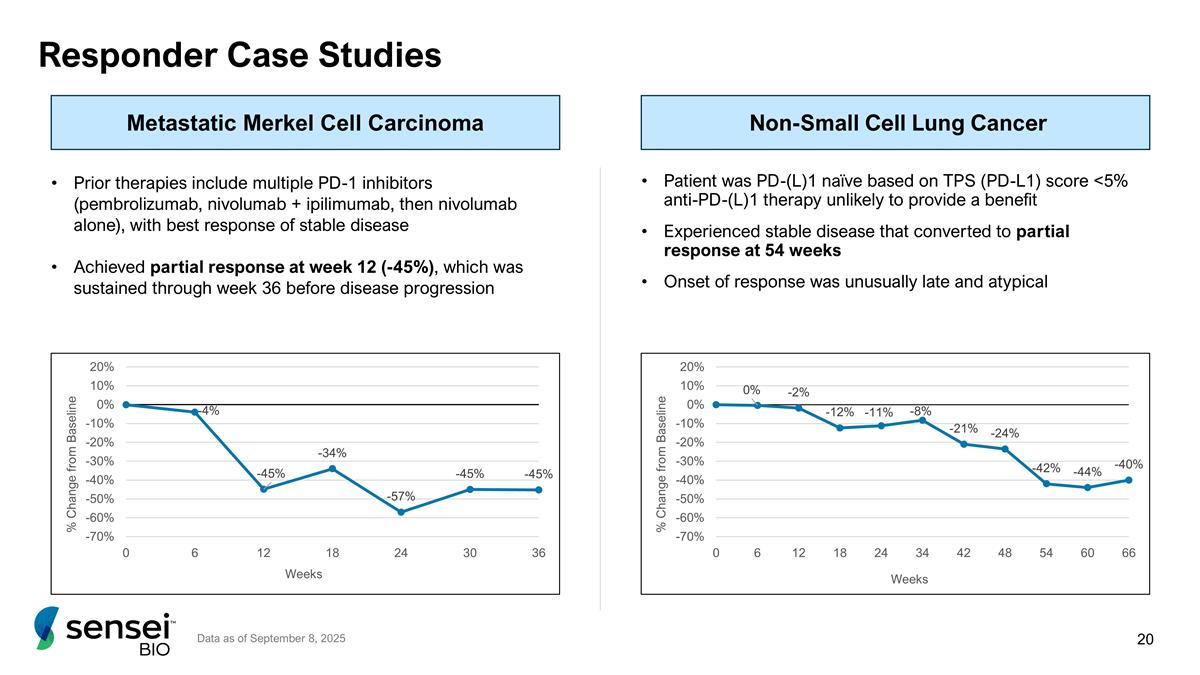
Responder Case Studies Prior therapies include multiple PD-1 inhibitors (pembrolizumab, nivolumab + ipilimumab, then nivolumab alone), with best response of stable disease Achieved partial response at week 12 (-45%), which was sustained through week 36 before disease progression Patient was PD-(L)1 naïve based on TPS (PD-L1) score <5% anti-PD-(L)1 therapy unlikely to provide a benefit Experienced stable disease that converted to partial response at 54 weeks Onset of response was unusually late and atypical Metastatic Merkel Cell Carcinoma Non-Small Cell Lung Cancer Data as of September 8, 2025
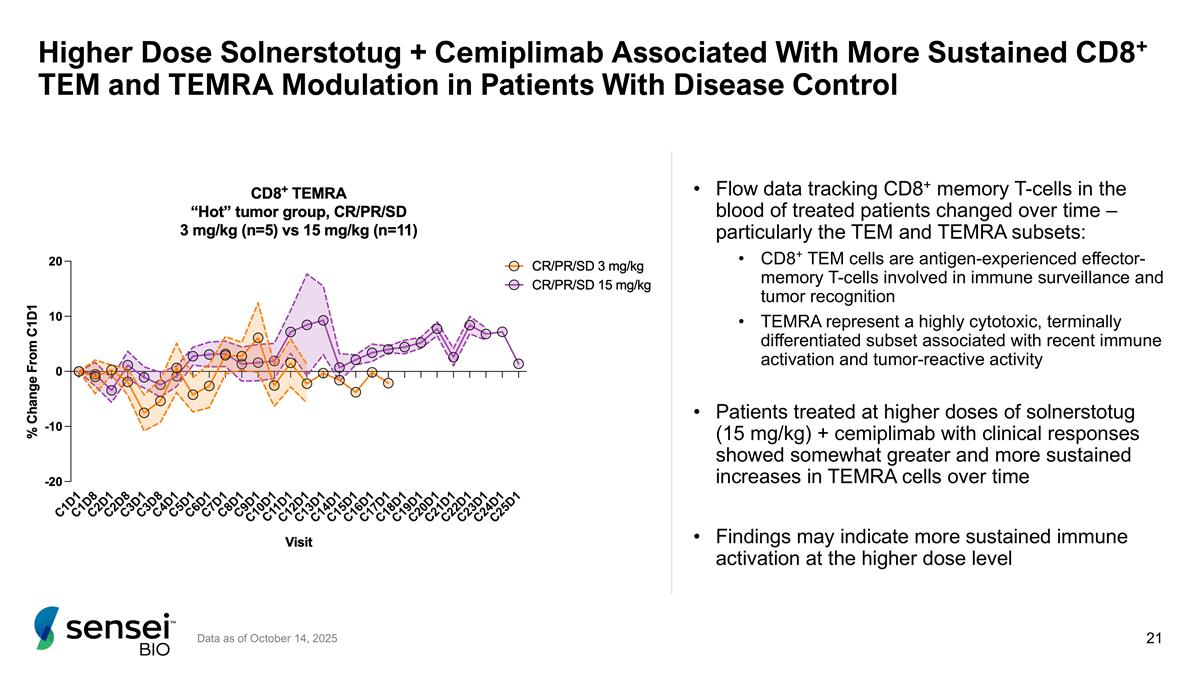
Higher Dose Solnerstotug + Cemiplimab Associated With More Sustained CD8+ TEM and TEMRA Modulation in Patients With Disease Control Flow data tracking CD8+ memory T-cells in the blood of treated patients changed over time – particularly the TEM and TEMRA subsets: CD8⁺ TEM cells are antigen-experienced effector-memory T-cells involved in immune surveillance and tumor recognition TEMRA represent a highly cytotoxic, terminally differentiated subset associated with recent immune activation and tumor-reactive activity Patients treated at higher doses of solnerstotug (15 mg/kg) + cemiplimab with clinical responses showed somewhat greater and more sustained increases in TEMRA cells over time Findings may indicate more sustained immune activation at the higher dose level Data as of October 14, 2025
Phase 1 Conclusions Solnerstotug/cemiplimab combination therapy demonstrates clinical activity in a PD-(L)1 resistant population of solid tumors: Durable clinical responses observed with a pattern of late onset response seen in 4 out of 5 patients Encouraging overall rate of PFS-6 of 37% Data suggests 15 mg/kg may have superior clinical activity All five responders were at this dose PFS-6 of 50% at this dose level All CRS events (Grade 1) occurred at this dose Data compares favorably to historical benchmarks in PD-(L)1 refractory settings Combination regimen shows acceptable safety and tolerability profile TEAE profile does not appear different than that of single agent cemiplimab CRS events were rare and low grade Combination with cemiplimab offers potential for generally well tolerated “all IO” doublet regimen where both agents may be administered until disease progression TEAE = treatment emergent adverse event PFS-6 = progression-free survival at 6 months
Rooted in key observations made with solnerstotug/cemiplimab combination in PD-(L)1 responsive cohort: Impressive/encouraging rates (PFS-6) of durable disease control over a broad range of solid tumor types Most of the objective responses are observed in the “hottest” of tumor types (Merkel Cell and MSI-High) and also saw durability in less “hot” tumor types Acceptable safety and tolerability profile for solnerstotug in combination with cemiplimab Basic assumptions incorporated into Phase 2 planning: Highest level of activity appears to be in the “hottest” tumor settings Level of activity observed with solnerstotug/cemiplimab may approximate the activity seen with ipilimumab/nivolumab doublet WITHOUT the severe toxicity associated with that doublet Late onset responses and durable stable disease suggest progression-free survival and possibly overall survival as appropriate endpoints going forward Indication selection balances a large commercial opportunity (NSCLC) with a fast-to-market opportunity (MCC) PFS-6 = progression-free survival at 6 months NSCLC = non-small cell lung cancer MCC = Merkel Cell carcinoma Phase 2 Strategy
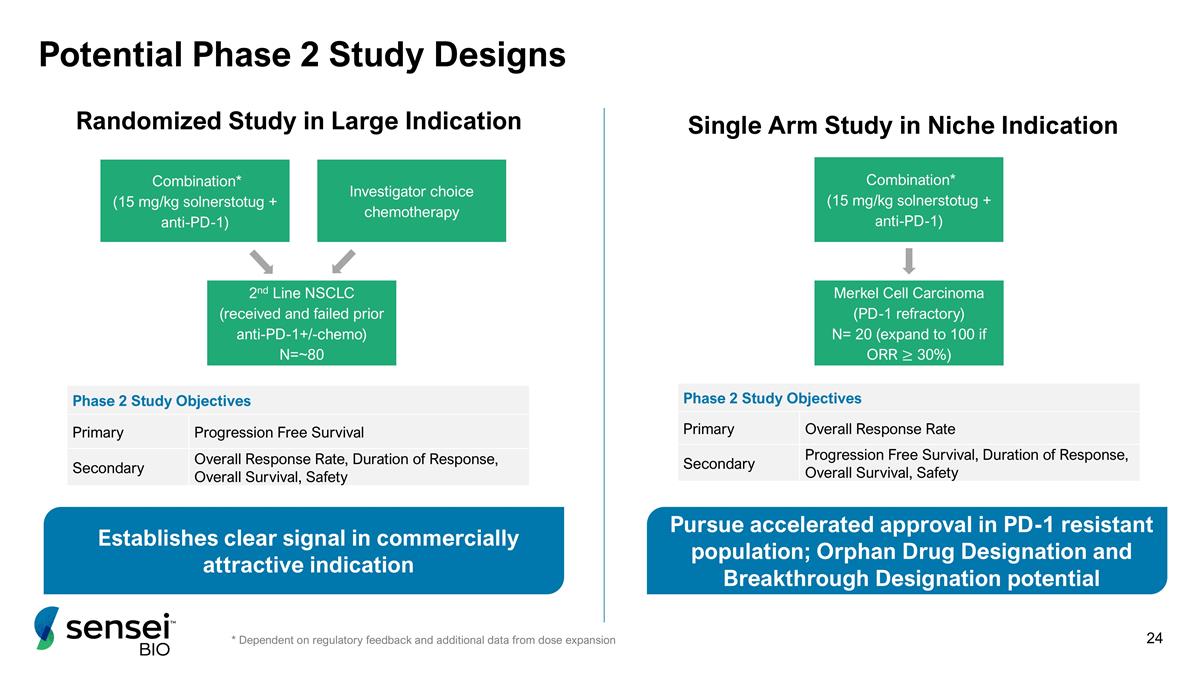
Potential Phase 2 Study Designs Randomized Study in Large Indication Single Arm Study in Niche Indication Combination* (15 mg/kg solnerstotug + anti-PD-1) Merkel Cell Carcinoma (PD-1 refractory) N= 20 (expand to 100 if ORR ≥ 30%) Phase 2 Study Objectives Primary Overall Response Rate Secondary Progression Free Survival, Duration of Response, Overall Survival, Safety Combination* (15 mg/kg solnerstotug + anti-PD-1) 2nd Line NSCLC (received and failed prior anti-PD-1+/-chemo) N=~80 Phase 2 Study Objectives Primary Progression Free Survival Secondary Overall Response Rate, Duration of Response, Overall Survival, Safety * Dependent on regulatory feedback and additional data from dose expansion Investigator choice chemotherapy Establishes clear signal in commercially attractive indication Pursue accelerated approval in PD-1 resistant population; Orphan Drug Designation and Breakthrough Designation potential
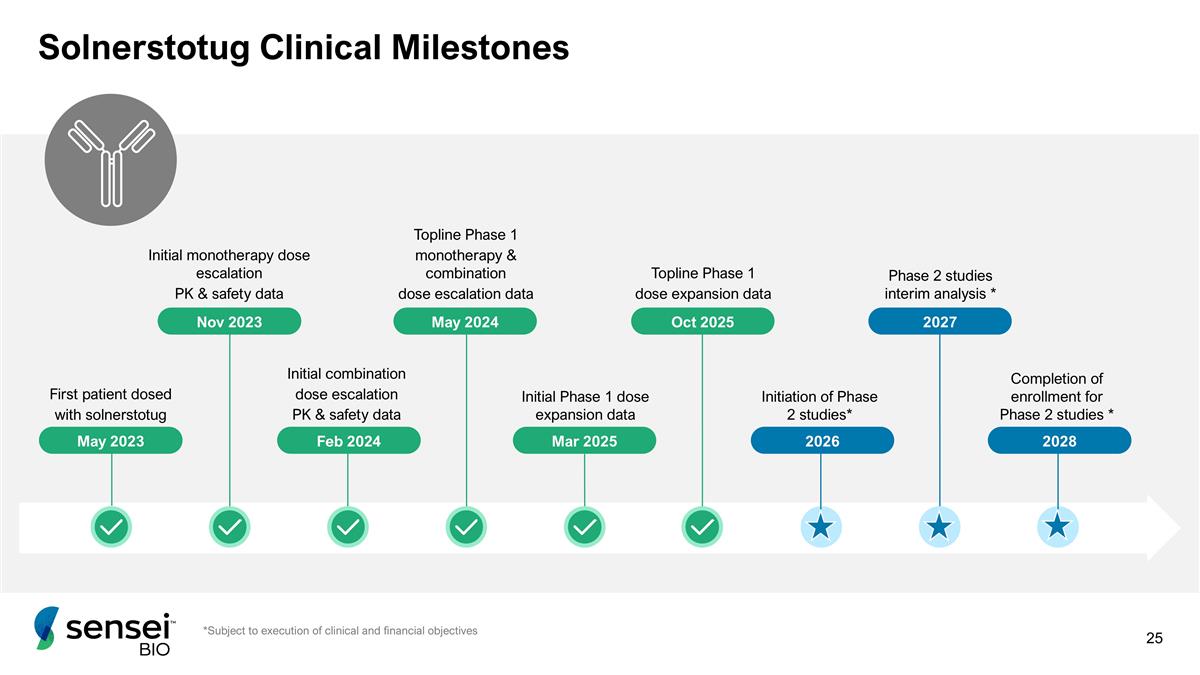
Solnerstotug Clinical Milestones Initial combination dose escalation PK & safety data First patient dosed with solnerstotug Initial monotherapy dose escalation PK & safety data Topline Phase 1 monotherapy & combination dose escalation data Nov 2023 May 2024 May 2023 Feb 2024 Mar 2025 Phase 2 studies interim analysis * 2027 *Subject to execution of clinical and financial objectives Initial Phase 1 dose expansion data 2026 Oct 2025 Topline Phase 1 dose expansion data Initiation of Phase 2 studies* 2028 Completion of enrollment for Phase 2 studies *
Appendix
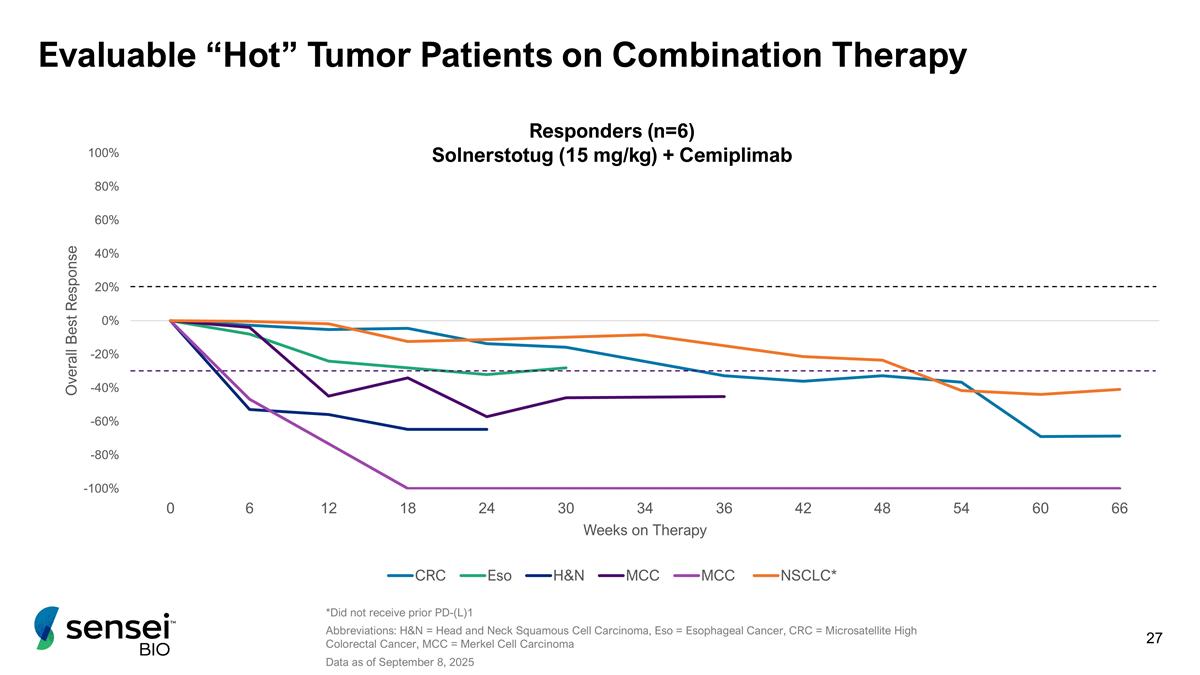
*Did not receive prior PD-(L)1 Abbreviations: H&N = Head and Neck Squamous Cell Carcinoma, Eso = Esophageal Cancer, CRC = Microsatellite High Colorectal Cancer, MCC = Merkel Cell Carcinoma Data as of September 8, 2025 Evaluable “Hot” Tumor Patients on Combination Therapy Responders (n=6) Solnerstotug (15 mg/kg) + Cemiplimab
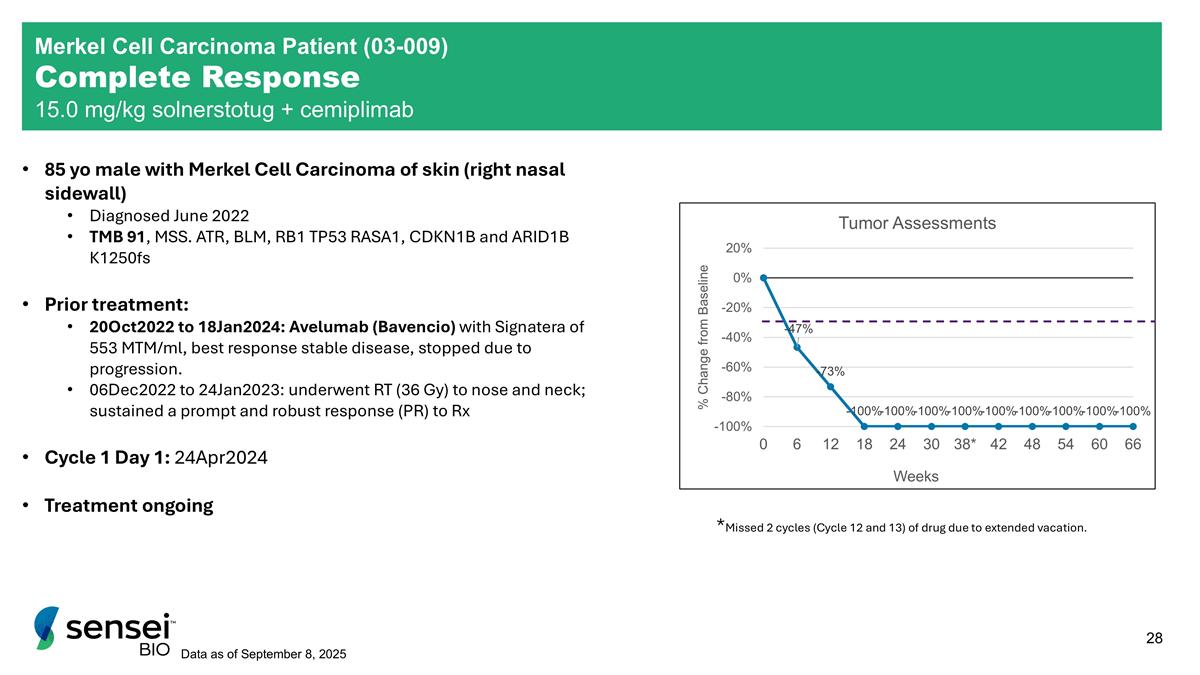
85 yo male with Merkel Cell Carcinoma of skin (right nasal sidewall) Diagnosed June 2022 TMB 91, MSS. ATR, BLM, RB1 TP53 RASA1, CDKN1B and ARID1B K1250fs Prior treatment: 20Oct2022 to 18Jan2024: Avelumab (Bavencio) with Signatera of 553 MTM/ml, best response stable disease, stopped due to progression. 06Dec2022 to 24Jan2023: underwent RT (36 Gy) to nose and neck; sustained a prompt and robust response (PR) to Rx Cycle 1 Day 1: 24Apr2024 Treatment ongoing *Missed 2 cycles (Cycle 12 and 13) of drug due to extended vacation. Data as of September 8, 2025 Merkel Cell Carcinoma Patient (03-009) Complete Response 15.0 mg/kg solnerstotug + cemiplimab
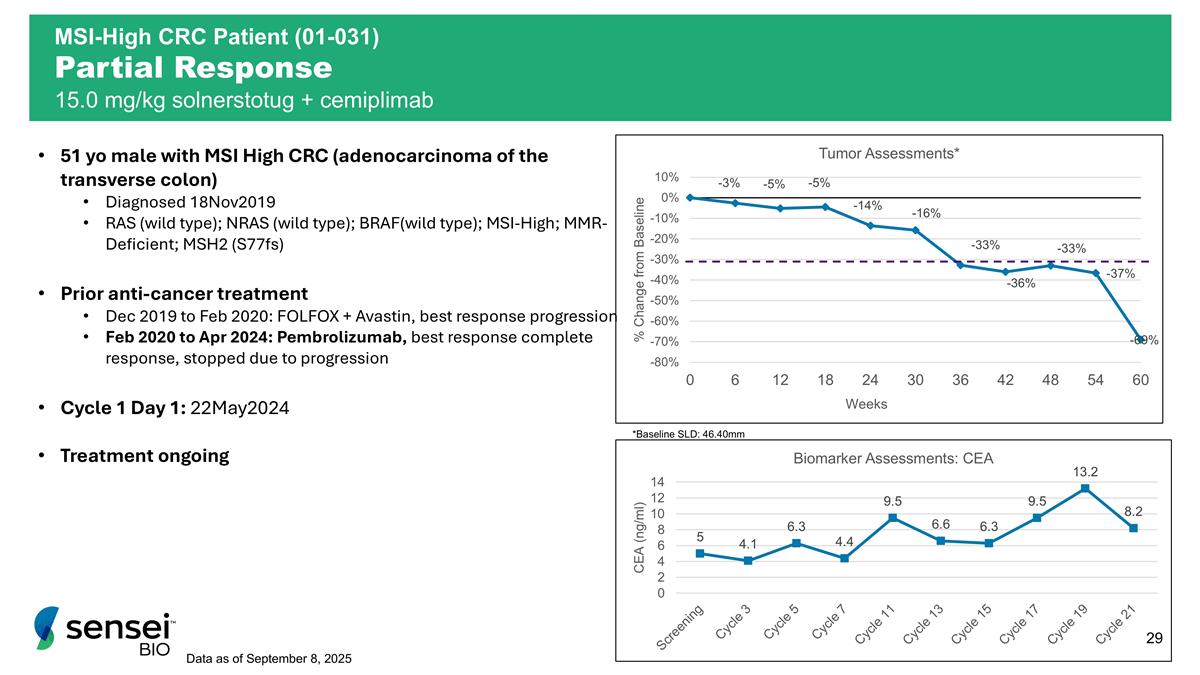
51 yo male with MSI High CRC (adenocarcinoma of the transverse colon) Diagnosed 18Nov2019 RAS (wild type); NRAS (wild type); BRAF(wild type); MSI-High; MMR- Deficient; MSH2 (S77fs) Prior anti-cancer treatment Dec 2019 to Feb 2020: FOLFOX + Avastin, best response progression Feb 2020 to Apr 2024: Pembrolizumab, best response complete response, stopped due to progression Cycle 1 Day 1: 22May2024 Treatment ongoing Data as of September 8, 2025 *Baseline SLD: 46.40mm MSI-High CRC Patient (01-031) Partial Response 15.0 mg/kg solnerstotug + cemiplimab
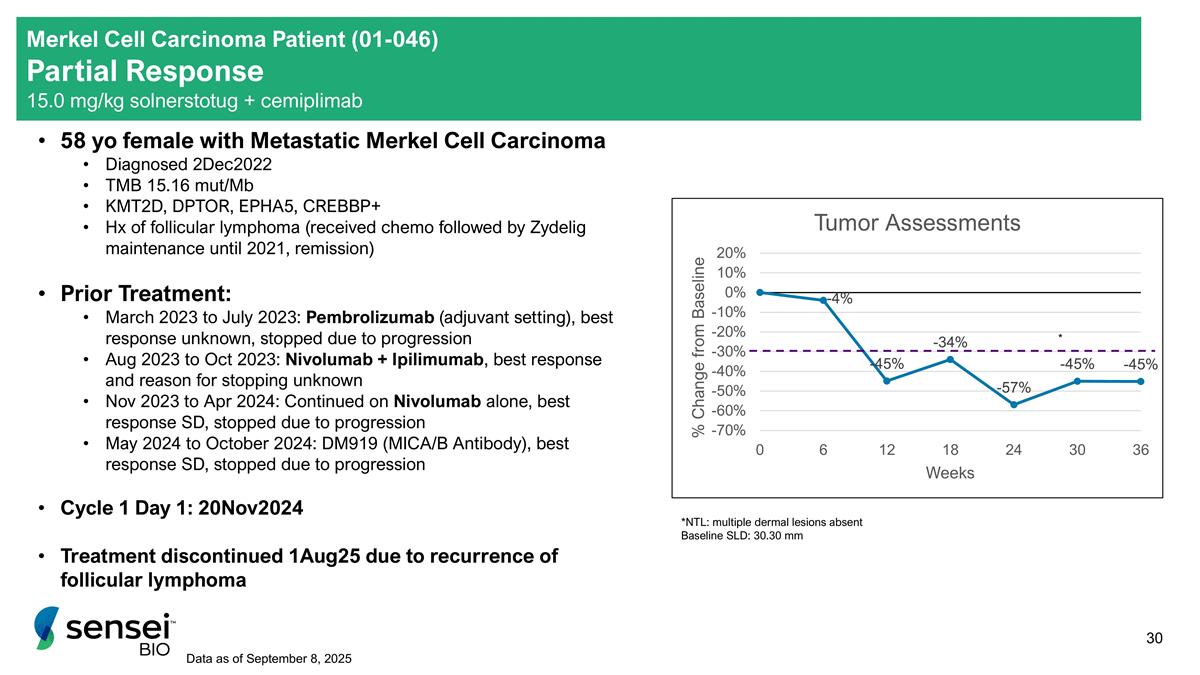
58 yo female with Metastatic Merkel Cell Carcinoma Diagnosed 2Dec2022 TMB 15.16 mut/Mb KMT2D, DPTOR, EPHA5, CREBBP+ Hx of follicular lymphoma (received chemo followed by Zydelig maintenance until 2021, remission) Prior Treatment: March 2023 to July 2023: Pembrolizumab (adjuvant setting), best response unknown, stopped due to progression Aug 2023 to Oct 2023: Nivolumab + Ipilimumab, best response and reason for stopping unknown Nov 2023 to Apr 2024: Continued on Nivolumab alone, best response SD, stopped due to progression May 2024 to October 2024: DM919 (MICA/B Antibody), best response SD, stopped due to progression Cycle 1 Day 1: 20Nov2024 Treatment discontinued 1Aug25 due to recurrence of follicular lymphoma *NTL: multiple dermal lesions absent Baseline SLD: 30.30 mm * Merkel Cell Carcinoma Patient (01-046) Partial Response 15.0 mg/kg solnerstotug + cemiplimab Data as of September 8, 2025
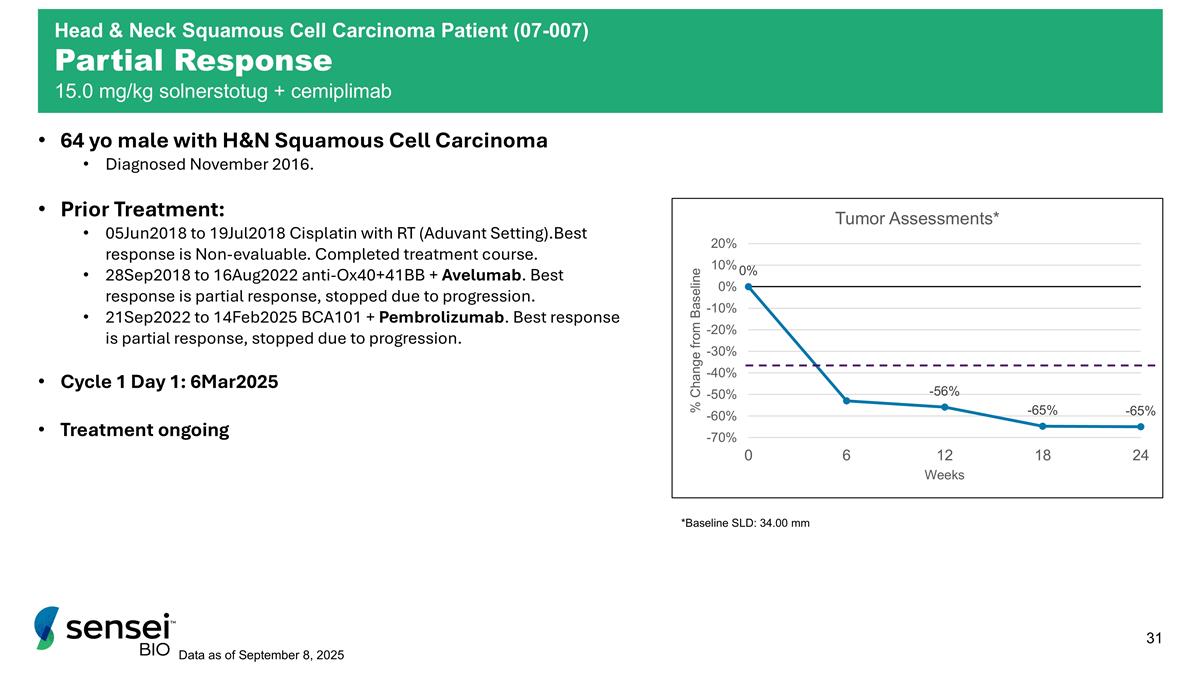
64 yo male with H&N Squamous Cell Carcinoma Diagnosed November 2016. Prior Treatment: 05Jun2018 to 19Jul2018 Cisplatin with RT (Aduvant Setting).Best response is Non-evaluable. Completed treatment course. 28Sep2018 to 16Aug2022 anti-Ox40+41BB + Avelumab. Best response is partial response, stopped due to progression. 21Sep2022 to 14Feb2025 BCA101 + Pembrolizumab. Best response is partial response, stopped due to progression. Cycle 1 Day 1: 6Mar2025 Treatment ongoing Data as of September 8, 2025 *Baseline SLD: 34.00 mm Head & Neck Squamous Cell Carcinoma Patient (07-007) Partial Response 15.0 mg/kg solnerstotug + cemiplimab
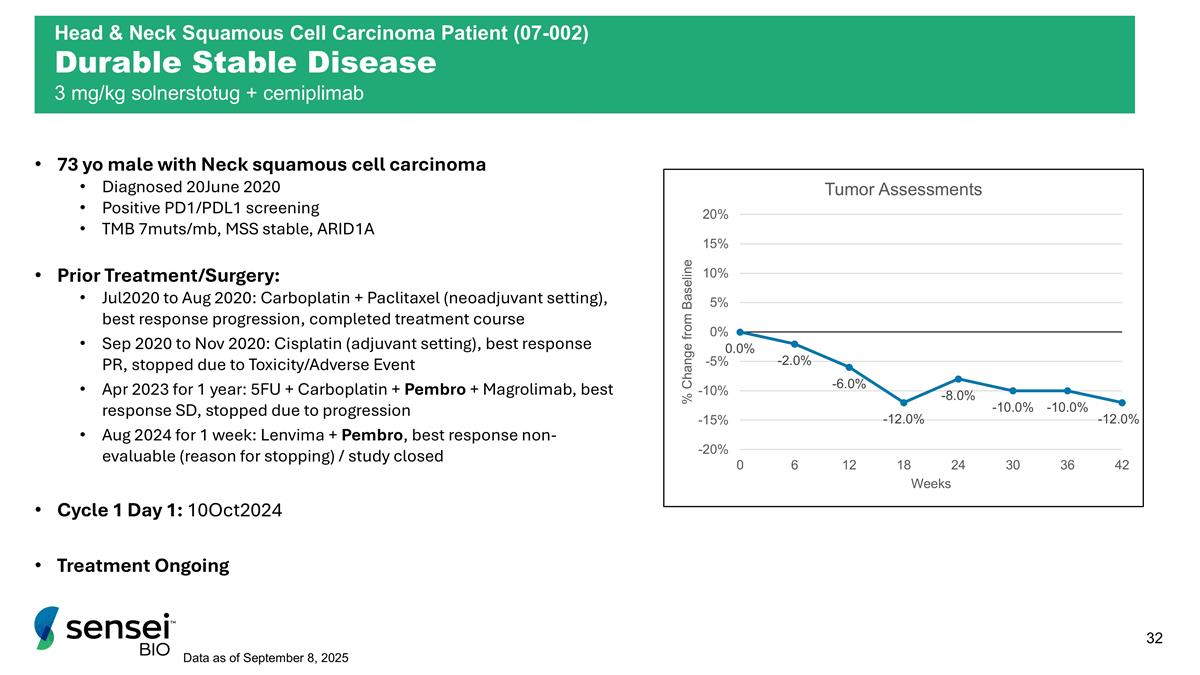
73 yo male with Neck squamous cell carcinoma Diagnosed 20June 2020 Positive PD1/PDL1 screening TMB 7muts/mb, MSS stable, ARID1A Prior Treatment/Surgery: Jul2020 to Aug 2020: Carboplatin + Paclitaxel (neoadjuvant setting), best response progression, completed treatment course Sep 2020 to Nov 2020: Cisplatin (adjuvant setting), best response PR, stopped due to Toxicity/Adverse Event Apr 2023 for 1 year: 5FU + Carboplatin + Pembro + Magrolimab, best response SD, stopped due to progression Aug 2024 for 1 week: Lenvima + Pembro, best response non-evaluable (reason for stopping) / study closed Cycle 1 Day 1: 10Oct2024 Treatment Ongoing Data as of September 8, 2025 Head & Neck Squamous Cell Carcinoma Patient (07-002) Durable Stable Disease 3 mg/kg solnerstotug + cemiplimab
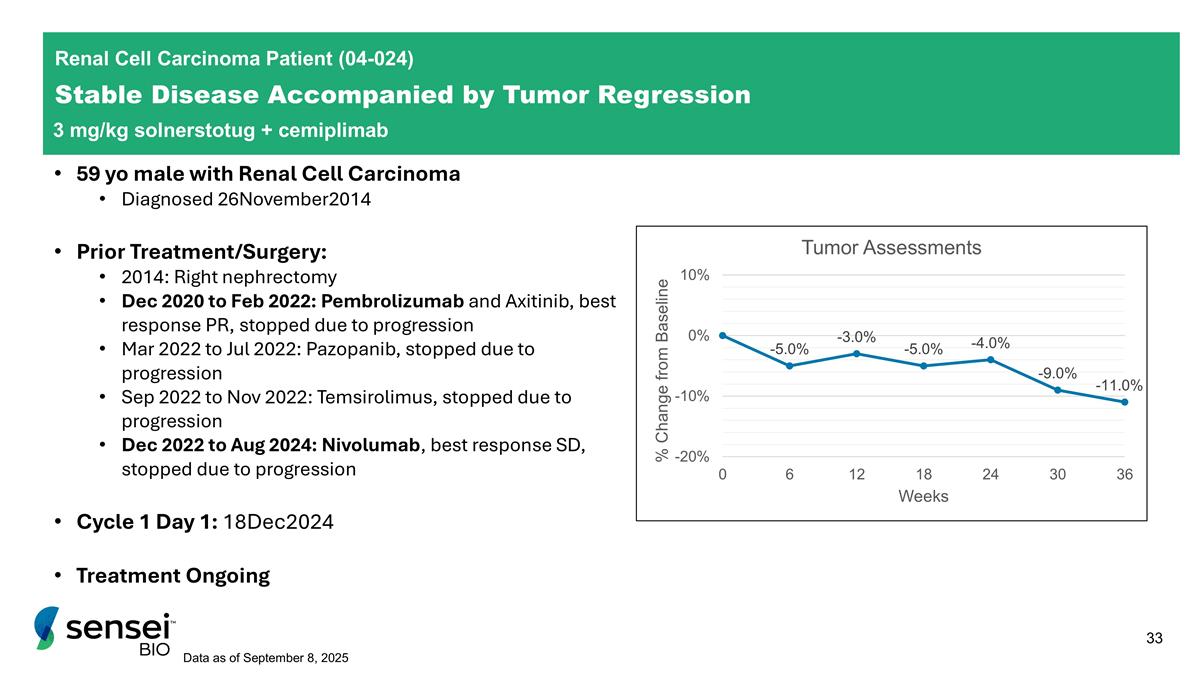
Renal Cell Carcinoma Patient (04-024) Stable Disease Accompanied by Tumor Regression 3 mg/kg solnerstotug + cemiplimab 59 yo male with Renal Cell Carcinoma Diagnosed 26November2014 Prior Treatment/Surgery: 2014: Right nephrectomy Dec 2020 to Feb 2022: Pembrolizumab and Axitinib, best response PR, stopped due to progression Mar 2022 to Jul 2022: Pazopanib, stopped due to progression Sep 2022 to Nov 2022: Temsirolimus, stopped due to progression Dec 2022 to Aug 2024: Nivolumab, best response SD, stopped due to progression Cycle 1 Day 1: 18Dec2024 Treatment Ongoing Data as of September 8, 2025
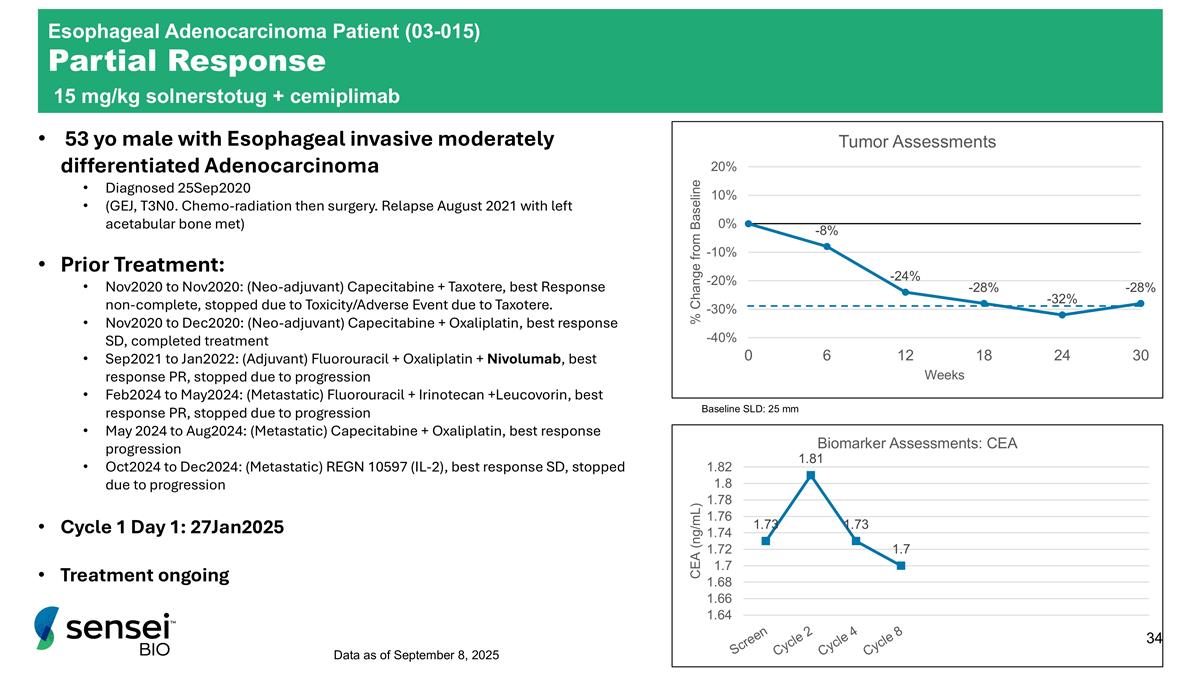
Esophageal Adenocarcinoma Patient (03-015) Partial Response 15 mg/kg solnerstotug + cemiplimab 53 yo male with Esophageal invasive moderately differentiated Adenocarcinoma Diagnosed 25Sep2020 (GEJ, T3N0. Chemo-radiation then surgery. Relapse August 2021 with left acetabular bone met) Prior Treatment: Nov2020 to Nov2020: (Neo-adjuvant) Capecitabine + Taxotere, best Response non-complete, stopped due to Toxicity/Adverse Event due to Taxotere. Nov2020 to Dec2020: (Neo-adjuvant) Capecitabine + Oxaliplatin, best response SD, completed treatment Sep2021 to Jan2022: (Adjuvant) Fluorouracil + Oxaliplatin + Nivolumab, best response PR, stopped due to progression Feb2024 to May2024: (Metastatic) Fluorouracil + Irinotecan +Leucovorin, best response PR, stopped due to progression May 2024 to Aug2024: (Metastatic) Capecitabine + Oxaliplatin, best response progression Oct2024 to Dec2024: (Metastatic) REGN 10597 (IL-2), best response SD, stopped due to progression Cycle 1 Day 1: 27Jan2025 Treatment ongoing Data as of September 8, 2025 Baseline SLD: 25 mm
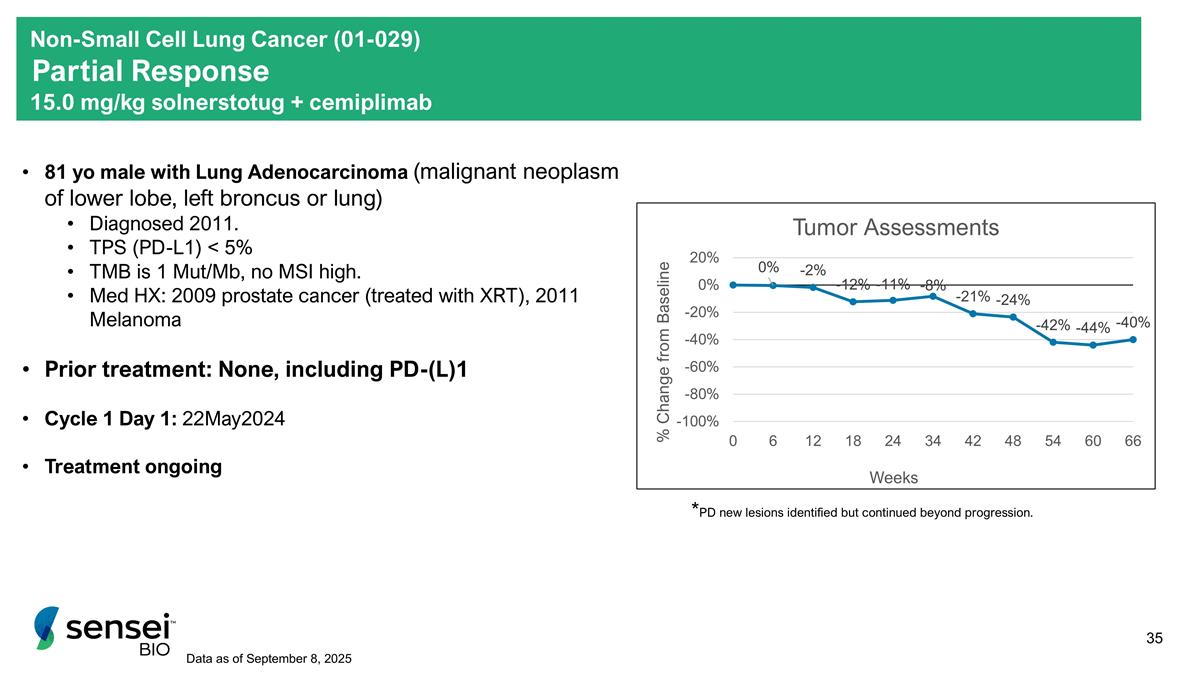
Non-Small Cell Lung Cancer (01-029) Partial Response 15.0 mg/kg solnerstotug + cemiplimab 81 yo male with Lung Adenocarcinoma (malignant neoplasm of lower lobe, left broncus or lung) Diagnosed 2011. TPS (PD-L1) < 5% TMB is 1 Mut/Mb, no MSI high. Med HX: 2009 prostate cancer (treated with XRT), 2011 Melanoma Prior treatment: None, including PD-(L)1 Cycle 1 Day 1: 22May2024 Treatment ongoing *PD new lesions identified but continued beyond progression. Data as of September 8, 2025
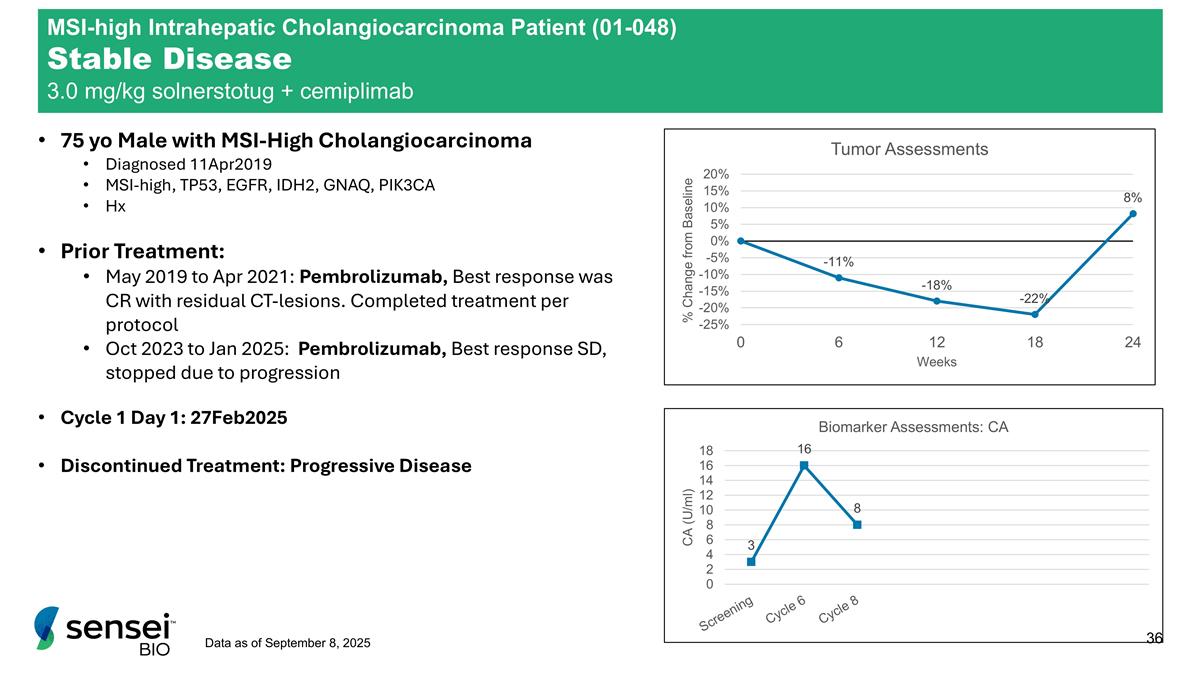
75 yo Male with MSI-High Cholangiocarcinoma Diagnosed 11Apr2019 MSI-high, TP53, EGFR, IDH2, GNAQ, PIK3CA Hx Prior Treatment: May 2019 to Apr 2021: Pembrolizumab, Best response was CR with residual CT-lesions. Completed treatment per protocol Oct 2023 to Jan 2025: Pembrolizumab, Best response SD, stopped due to progression Cycle 1 Day 1: 27Feb2025 Discontinued Treatment: Progressive Disease Data as of September 8, 2025 MSI-high Intrahepatic Cholangiocarcinoma Patient (01-048) Stable Disease 3.0 mg/kg solnerstotug + cemiplimab
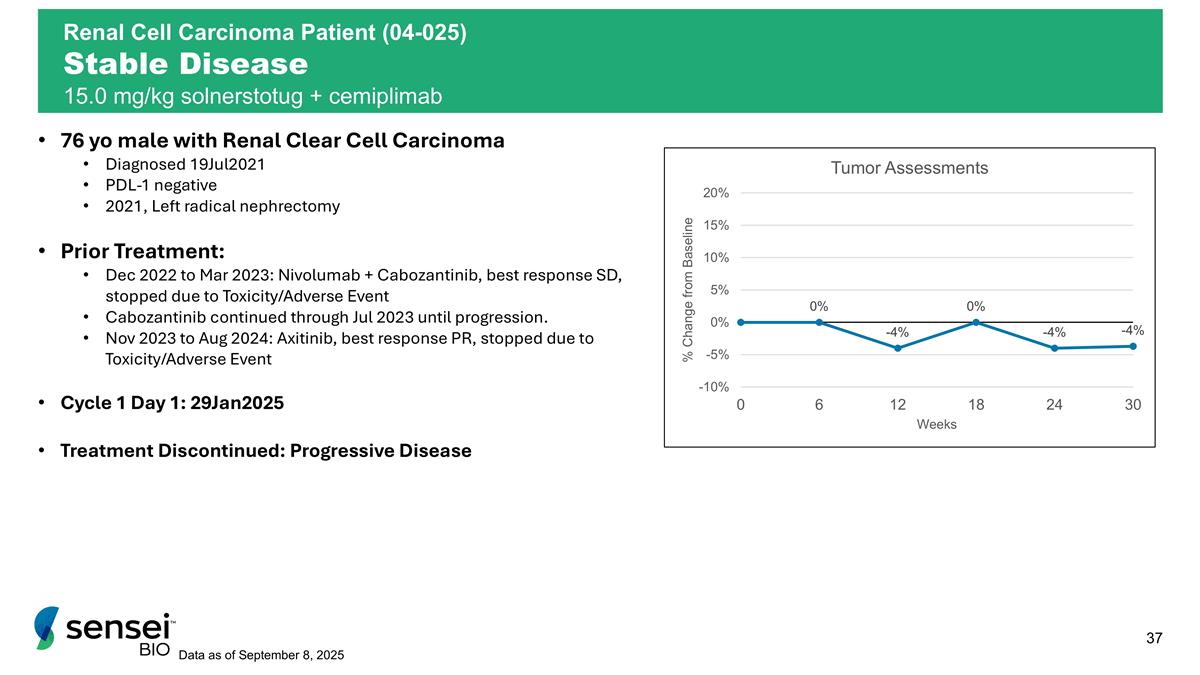
76 yo male with Renal Clear Cell Carcinoma Diagnosed 19Jul2021 PDL-1 negative 2021, Left radical nephrectomy Prior Treatment: Dec 2022 to Mar 2023: Nivolumab + Cabozantinib, best response SD, stopped due to Toxicity/Adverse Event Cabozantinib continued through Jul 2023 until progression. Nov 2023 to Aug 2024: Axitinib, best response PR, stopped due to Toxicity/Adverse Event Cycle 1 Day 1: 29Jan2025 Treatment Discontinued: Progressive Disease Data as of September 8, 2025 Renal Cell Carcinoma Patient (04-025) Stable Disease 15.0 mg/kg solnerstotug + cemiplimab
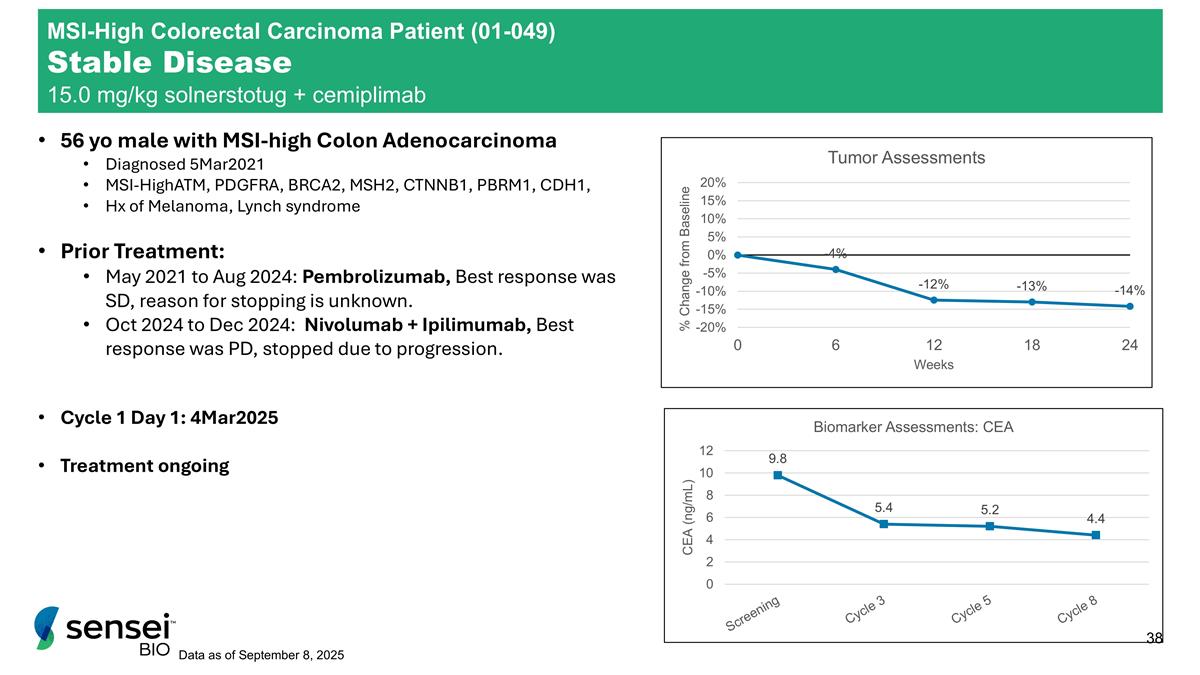
56 yo male with MSI-high Colon Adenocarcinoma Diagnosed 5Mar2021 MSI-HighATM, PDGFRA, BRCA2, MSH2, CTNNB1, PBRM1, CDH1, Hx of Melanoma, Lynch syndrome Prior Treatment: May 2021 to Aug 2024: Pembrolizumab, Best response was SD, reason for stopping is unknown. Oct 2024 to Dec 2024: Nivolumab + Ipilimumab, Best response was PD, stopped due to progression. Cycle 1 Day 1: 4Mar2025 Treatment ongoing Data as of September 8, 2025 MSI-High Colorectal Carcinoma Patient (01-049) Stable Disease 15.0 mg/kg solnerstotug + cemiplimab
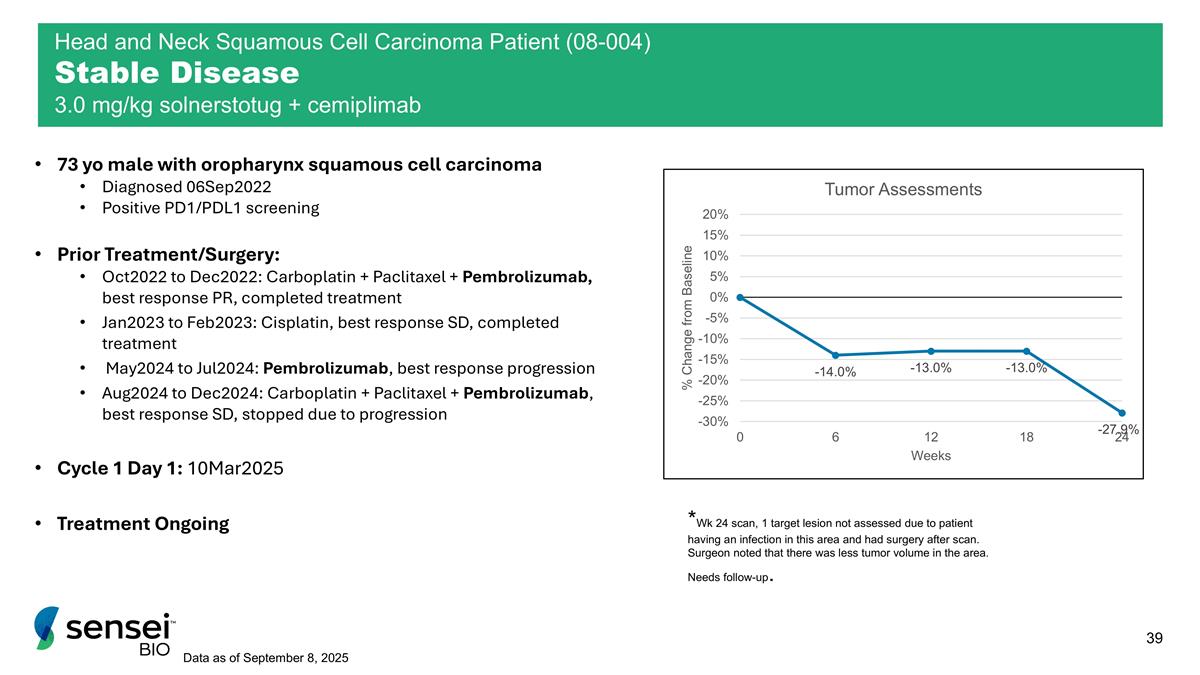
73 yo male with oropharynx squamous cell carcinoma Diagnosed 06Sep2022 Positive PD1/PDL1 screening Prior Treatment/Surgery: Oct2022 to Dec2022: Carboplatin + Paclitaxel + Pembrolizumab, best response PR, completed treatment Jan2023 to Feb2023: Cisplatin, best response SD, completed treatment May2024 to Jul2024: Pembrolizumab, best response progression Aug2024 to Dec2024: Carboplatin + Paclitaxel + Pembrolizumab, best response SD, stopped due to progression Cycle 1 Day 1: 10Mar2025 Treatment Ongoing Data as of September 8, 2025 Head and Neck Squamous Cell Carcinoma Patient (08-004) Stable Disease 3.0 mg/kg solnerstotug + cemiplimab *Wk 24 scan, 1 target lesion not assessed due to patient having an infection in this area and had surgery after scan. Surgeon noted that there was less tumor volume in the area. Needs follow-up.
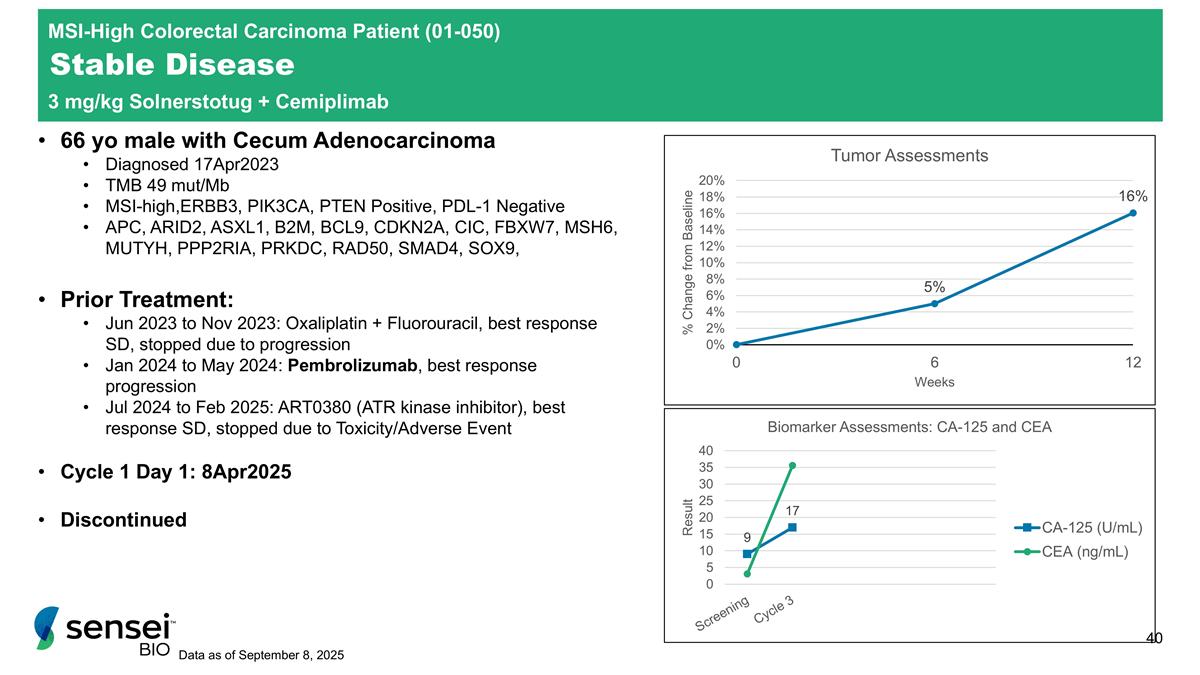
MSI-High Colorectal Carcinoma Patient (01-050) Stable Disease 3 mg/kg Solnerstotug + Cemiplimab 66 yo male with Cecum Adenocarcinoma Diagnosed 17Apr2023 TMB 49 mut/Mb MSI-high,ERBB3, PIK3CA, PTEN Positive, PDL-1 Negative APC, ARID2, ASXL1, B2M, BCL9, CDKN2A, CIC, FBXW7, MSH6, MUTYH, PPP2RIA, PRKDC, RAD50, SMAD4, SOX9, Prior Treatment: Jun 2023 to Nov 2023: Oxaliplatin + Fluorouracil, best response SD, stopped due to progression Jan 2024 to May 2024: Pembrolizumab, best response progression Jul 2024 to Feb 2025: ART0380 (ATR kinase inhibitor), best response SD, stopped due to Toxicity/Adverse Event Cycle 1 Day 1: 8Apr2025 Discontinued Data as of September 8, 2025
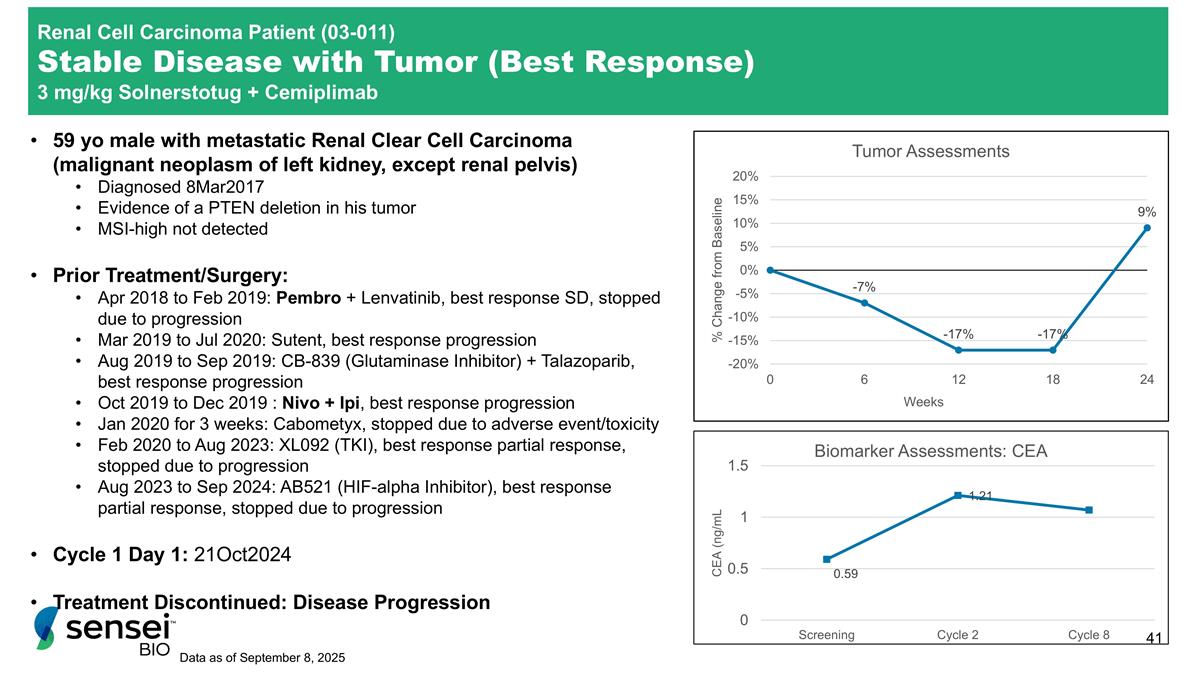
59 yo male with metastatic Renal Clear Cell Carcinoma (malignant neoplasm of left kidney, except renal pelvis) Diagnosed 8Mar2017 Evidence of a PTEN deletion in his tumor MSI-high not detected Prior Treatment/Surgery: Apr 2018 to Feb 2019: Pembro + Lenvatinib, best response SD, stopped due to progression Mar 2019 to Jul 2020: Sutent, best response progression Aug 2019 to Sep 2019: CB-839 (Glutaminase Inhibitor) + Talazoparib, best response progression Oct 2019 to Dec 2019 : Nivo + Ipi, best response progression Jan 2020 for 3 weeks: Cabometyx, stopped due to adverse event/toxicity Feb 2020 to Aug 2023: XL092 (TKI), best response partial response, stopped due to progression Aug 2023 to Sep 2024: AB521 (HIF-alpha Inhibitor), best response partial response, stopped due to progression Cycle 1 Day 1: 21Oct2024 Treatment Discontinued: Disease Progression Data as of September 8, 2025 Renal Cell Carcinoma Patient (03-011) Stable Disease with Tumor (Best Response) 3 mg/kg Solnerstotug + Cemiplimab
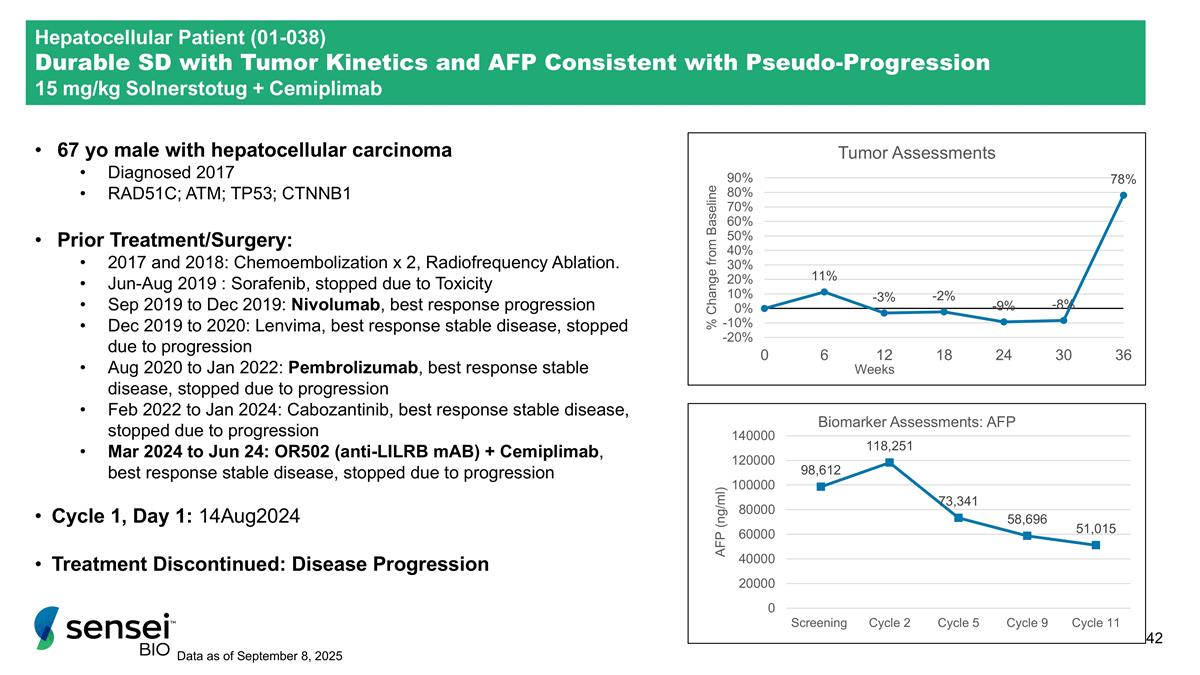
Hepatocellular Patient (01-038) Durable SD with Tumor Kinetics and AFP Consistent with Pseudo-Progression 15 mg/kg Solnerstotug + Cemiplimab 67 yo male with hepatocellular carcinoma Diagnosed 2017 RAD51C; ATM; TP53; CTNNB1 Prior Treatment/Surgery: 2017 and 2018: Chemoembolization x 2, Radiofrequency Ablation. Jun-Aug 2019 : Sorafenib, stopped due to Toxicity Sep 2019 to Dec 2019: Nivolumab, best response progression Dec 2019 to 2020: Lenvima, best response stable disease, stopped due to progression Aug 2020 to Jan 2022: Pembrolizumab, best response stable disease, stopped due to progression Feb 2022 to Jan 2024: Cabozantinib, best response stable disease, stopped due to progression Mar 2024 to Jun 24: OR502 (anti-LILRB mAB) + Cemiplimab, best response stable disease, stopped due to progression Cycle 1, Day 1: 14Aug2024 Treatment Discontinued: Disease Progression Data as of September 8, 2025
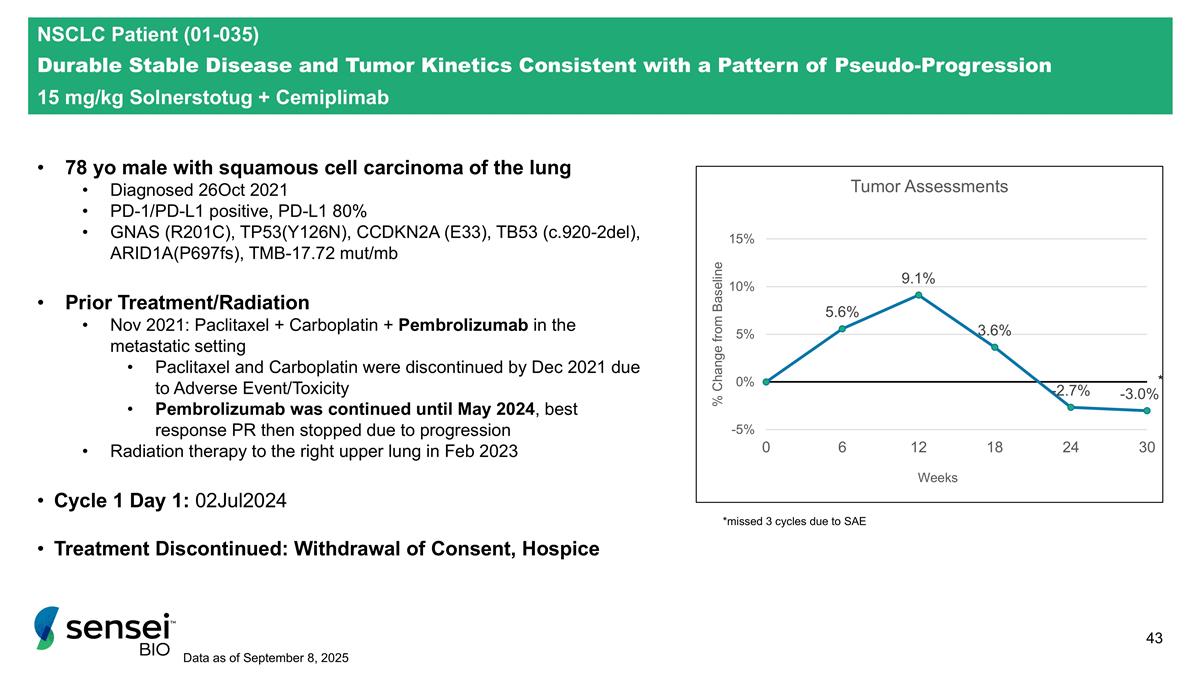
78 yo male with squamous cell carcinoma of the lung Diagnosed 26Oct 2021 PD-1/PD-L1 positive, PD-L1 80% GNAS (R201C), TP53(Y126N), CCDKN2A (E33), TB53 (c.920-2del), ARID1A(P697fs), TMB-17.72 mut/mb Prior Treatment/Radiation Nov 2021: Paclitaxel + Carboplatin + Pembrolizumab in the metastatic setting Paclitaxel and Carboplatin were discontinued by Dec 2021 due to Adverse Event/Toxicity Pembrolizumab was continued until May 2024, best response PR then stopped due to progression Radiation therapy to the right upper lung in Feb 2023 Cycle 1 Day 1: 02Jul2024 Treatment Discontinued: Withdrawal of Consent, Hospice NSCLC Patient (01-035) Durable Stable Disease and Tumor Kinetics Consistent with a Pattern of Pseudo-Progression 15 mg/kg Solnerstotug + Cemiplimab Data as of September 8, 2025 *missed 3 cycles due to SAE
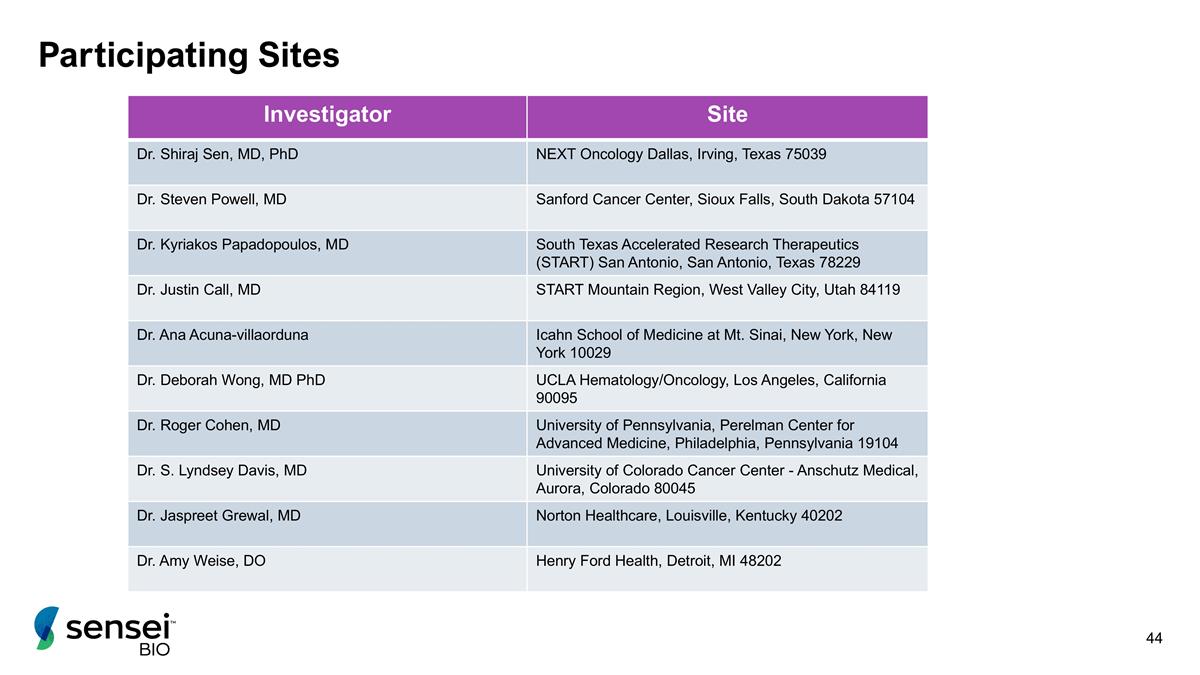
Participating Sites Investigator Site Dr. Shiraj Sen, MD, PhD NEXT Oncology Dallas, Irving, Texas 75039 Dr. Steven Powell, MD Sanford Cancer Center, Sioux Falls, South Dakota 57104 Dr. Kyriakos Papadopoulos, MD South Texas Accelerated Research Therapeutics (START) San Antonio, San Antonio, Texas 78229 Dr. Justin Call, MD START Mountain Region, West Valley City, Utah 84119 Dr. Ana Acuna-villaorduna Icahn School of Medicine at Mt. Sinai, New York, New York 10029 Dr. Deborah Wong, MD PhD UCLA Hematology/Oncology, Los Angeles, California 90095 Dr. Roger Cohen, MD University of Pennsylvania, Perelman Center for Advanced Medicine, Philadelphia, Pennsylvania 19104 Dr. S. Lyndsey Davis, MD University of Colorado Cancer Center - Anschutz Medical, Aurora, Colorado 80045 Dr. Jaspreet Grewal, MD Norton Healthcare, Louisville, Kentucky 40202 Dr. Amy Weise, DO Henry Ford Health, Detroit, MI 48202

MD: 1405 Research Blvd, Suite 125, Rockville, MD 20850 / MA: 451 D Street, Suite 906, Boston, MA 02210 senseibio.com