

.2 Day One Biopharmaceuticals Targeted therapies for people of all ages November 2025
Disclaimer This presentation and the accompanying oral commentary contain forward-looking statements that are based on our management’s beliefs and assumptions and on information currently available to our management. Forward-looking statements are inherently subject to risks and uncertainties, some of which cannot be predicted or quantified. In some cases, you can identify forward-looking statements by terminology such as “may,” “will,” “should,” “could,” “expect,” “plan,” anticipate,” “believe,” “estimate,” “predict,” “intend,” “potential,” “would,” “continue,” “ongoing” or the negative of these terms or other comparable terminology. Forward-looking statements include all statements other than statements of historical fact contained in this presentation, including information concerning our future financial performance, including the sufficiency of our cash, cash equivalents and short-term investments to fund our operations, business plans and objectives, timing and success of our commercialization and marketing efforts, timing and success of our planned nonclinical and clinical development activities, the success of our proposed acquisition of Mersana Therapeutics and its Emi-Le program, the results of any of our strategic collaborations, including the potential achievement of milestones and provision of royalty payments thereunder, efficacy and safety profiles of our products and product candidates, the ability of OJEMDA (tovorafenib) to treat pediatric low-grade glioma (pLGG) or related indications, the potential therapeutic benefits and economic value of our products and product candidates, potential growth opportunities, competitive position, industry environment and potential market opportunities, our ability to protect intellectual property and the impact of global business or macroeconomic conditions, including as a result of inflation, changing interest rates, government shutdowns, cybersecurity incidents, significant political, trade or regulatory developments, including tariffs, shifting priorities within the U.S. Food and Drug Administration and reduced funding of federal healthcare programs, and global regional conflicts, on our business and operations. Forward-looking statements are subject to known and unknown risks, uncertainties, assumptions and other factors. It is not possible for our management to predict all risks, nor can we assess the impact of all factors on our business or the extent to which any factor, or combination of factors, may cause actual results to differ materially from those contained in any forward-looking statements we may make. These factors, together with those that are described under the heading “Risk Factors” contained in our most recent Quarterly Report on Form 10-Q filed with the Securities and Exchange Commission (SEC) and other documents we file from time to time with the SEC, may cause our actual results, performance or achievements to differ materially and adversely from those anticipated or implied by our forward-looking statements. In addition, statements that “we believe” and similar statements reflect our beliefs and opinions on the relevant subject. These statements are based upon information available to us as of the date of this presentation, and although we believe such information forms a reasonable basis for such statements, such information may be limited or incomplete, and our statements should not be read to indicate that we have conducted a thorough inquiry into, or review of, all potentially available relevant information. These statements are inherently uncertain and investors are cautioned not to unduly rely upon these statements. Furthermore, if our forward-looking statements prove to be inaccurate, the inaccuracy may be material. In light of the significant uncertainties in these forward-looking statements, you should not regard these statements as a representation or warranty by us or any other person that we will achieve our objectives and plans in any specified time frame, or at all. We undertake no obligation to publicly update any forward-looking statements, whether as a result of new information, future events or otherwise, except as required by law. This presentation also contains estimates and other statistical data made by independent parties and by us relating to market size and growth and other data about our industry. This data involves a number of assumptions and limitations, and you are cautioned not to give undue weight to such estimates. In addition, projections, assumptions and estimates of our future performance and the future performance of the markets in which we operate are necessarily subject to a high degree of uncertainty and risk. 2

Inspired by the urgent needs of children, Day One creatively and intentionally develops new medicines for people of all ages with life- threatening diseases 3
Bringing life-changing medicines to patients sooner Who we are • Commercial-stage biopharmaceutical company • Our goal is to develop and provide access to targeted new medicines to patients of all ages as rapidly as possible • Focused on advancing first- or best-in-class medicines for childhood and adult diseases 2018 2021 2024 TM OJEMDA FOUNDED IPO APPROVAL Nasdaq: DAWN OJEMDA received approval in April 2024 and is indicated for the treatment of pediatric patients 6 months of age and older with relapsed or refractory pediatric low-grade glioma harboring a BRAF 4 fusion or rearrangement, or BRAF V600 mutation.
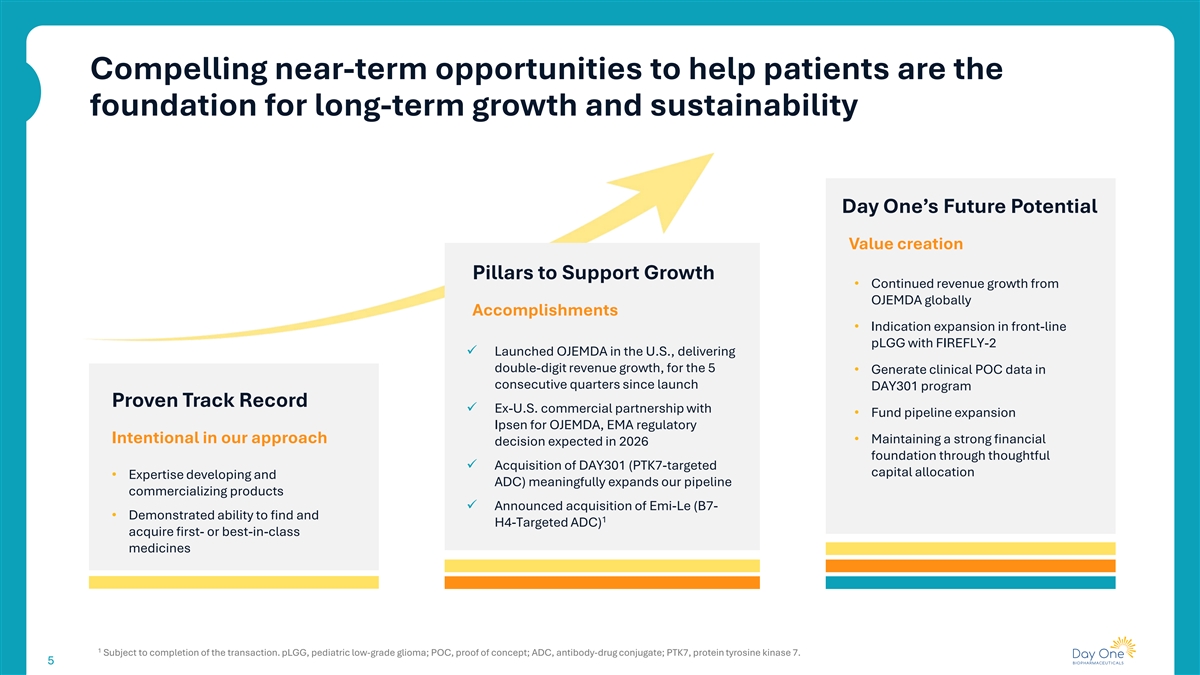
Compelling near-term opportunities to help patients are the foundation for long-term growth and sustainability Day One’s Future Potential Value creation Pillars to Support Growth • Continued revenue growth from OJEMDA globally Accomplishments • Indication expansion in front-line pLGG with FIREFLY-2 ü Launched OJEMDA in the U.S., delivering double-digit revenue growth, for the 5 • Generate clinical POC data in consecutive quarters since launch DAY301 program Proven Track Record ü Ex-U.S. commercial partnership with • Fund pipeline expansion Ipsen for OJEMDA, EMA regulatory Intentional in our approach • Maintaining a strong financial decision expected in 2026 foundation through thoughtful ü Acquisition of DAY301 (PTK7-targeted capital allocation • Expertise developing and ADC) meaningfully expands our pipeline commercializing products ü Announced acquisition of Emi-Le (B7- • Demonstrated ability to find and 1 H4-Targeted ADC) acquire first- or best-in-class medicines 1 Subject to completion of the transaction. pLGG, pediatric low-grade glioma; POC, proof of concept; ADC, antibody-drug conjugate; PTK7, protein tyrosine kinase 7. 5 5
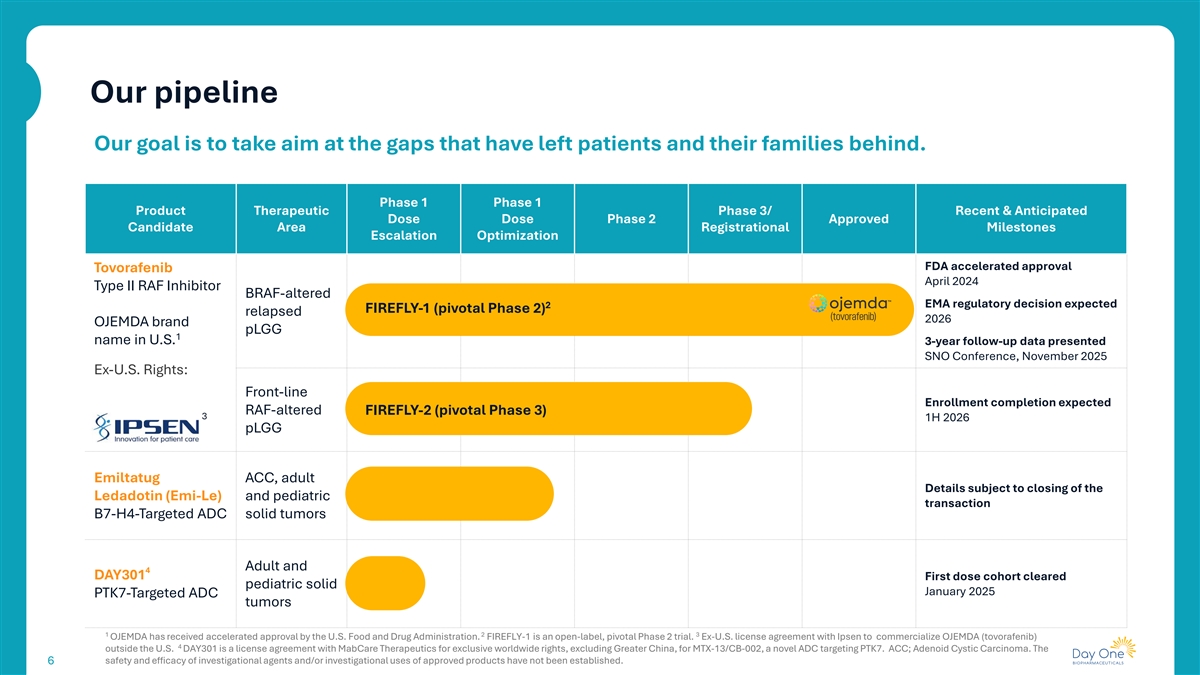
Our pipeline Our goal is to take aim at the gaps that have left patients and their families behind. Phase 1 Phase 1 Product Therapeutic Phase 3/ Recent & Anticipated Dose Dose Phase 2 Approved Candidate Area Registrational Milestones Escalation Optimization FDA accelerated approval Tovorafenib April 2024 Type II RAF Inhibitor BRAF-altered EMA regulatory decision expected 2 FIREFLY-1 (pivotal Phase 2) relapsed 2026 OJEMDA brand pLGG 1 name in U.S. 3-year follow-up data presented SNO Conference, November 2025 Ex-U.S. Rights: Front-line Enrollment completion expected RAF-altered FIREFLY-2 (pivotal Phase 3) 3 1H 2026 pLGG Emiltatug ACC, adult Details subject to closing of the Ledadotin (Emi-Le) and pediatric transaction B7-H4-Targeted ADC solid tumors Adult and 4 DAY301 First dose cohort cleared pediatric solid January 2025 PTK7-Targeted ADC tumors 1 2 3 OJEMDA has received accelerated approval by the U.S. Food and Drug Administration. FIREFLY-1 is an open-label, pivotal Phase 2 trial. Ex-U.S. license agreement with Ipsen to commercialize OJEMDA (tovorafenib) 4 outside the U.S. DAY301 is a license agreement with MabCare Therapeutics for exclusive worldwide rights, excluding Greater China, for MTX-13/CB-002, a novel ADC targeting PTK7. ACC; Adenoid Cystic Carcinoma. The safety and efficacy of investigational agents and/or investigational uses of approved products have not been established. 6

OJEMDA Relapsed or refractory BRAF-altered pLGG Nora Living with pLGG 7
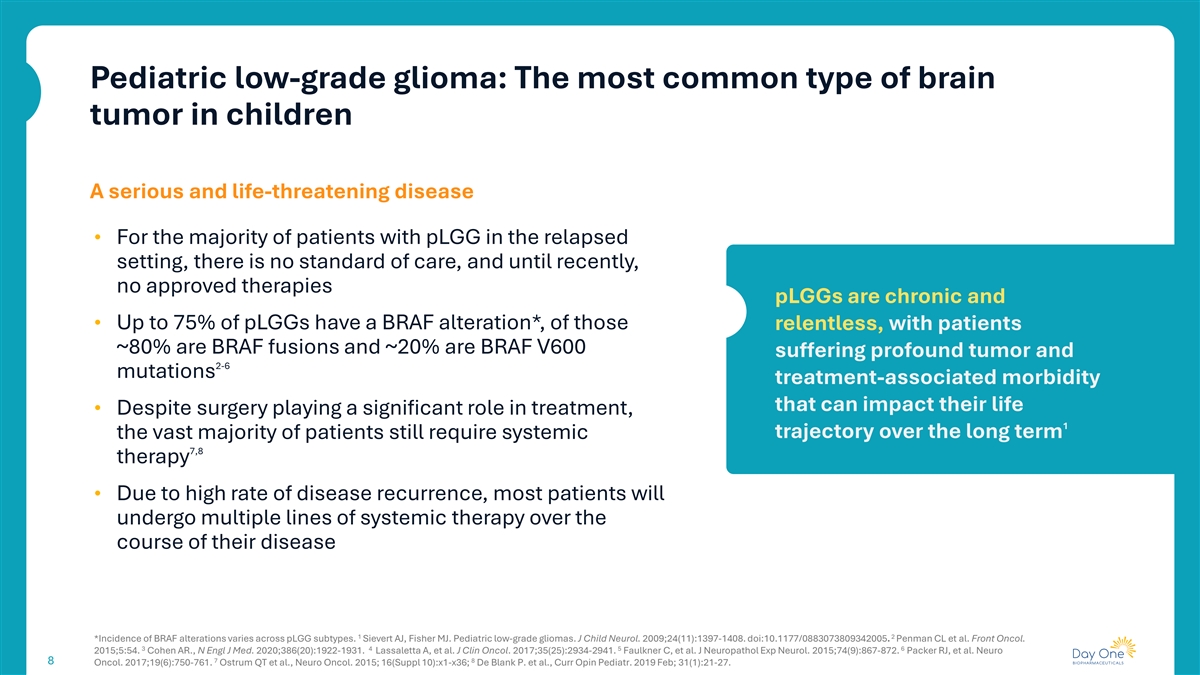
Pediatric low-grade glioma: The most common type of brain tumor in children A serious and life-threatening disease • For the majority of patients with pLGG in the relapsed setting, there is no standard of care, and until recently, no approved therapies pLGGs are chronic and • Up to 75% of pLGGs have a BRAF alteration*, of those relentless, with patients ~80% are BRAF fusions and ~20% are BRAF V600 suffering profound tumor and 2-6 mutations treatment-associated morbidity that can impact their life • Despite surgery playing a significant role in treatment, 1 the vast majority of patients still require systemic trajectory over the long term 7,8 therapy • Due to high rate of disease recurrence, most patients will undergo multiple lines of systemic therapy over the course of their disease 1 2 *Incidence of BRAF alterations varies across pLGG subtypes. Sievert AJ, Fisher MJ. Pediatric low-grade gliomas. J Child Neurol. 2009;24(11):1397-1408. doi:10.1177/0883073809342005. Penman CL et al. Front Oncol. 3 4 5 6 2015;5:54. Cohen AR., N Engl J Med. 2020;386(20):1922-1931. Lassaletta A, et al. J Clin Oncol. 2017;35(25):2934-2941. Faulkner C, et al. J Neuropathol Exp Neurol. 2015;74(9):867-872. Packer RJ, et al. Neuro 7 8 8 Oncol. 2017;19(6):750-761. Ostrum QT et al., Neuro Oncol. 2015; 16(Suppl 10):x1-x36; De Blank P. et al., Curr Opin Pediatr. 2019 Feb; 31(1):21-27.
Overview U.S. prescribing information for OJEMDA Available in tablet formulation and pediatric- friendly powder for oral suspension Indication OJEMDA is indicated for the treatment of pediatric patients 6 months of age and older with relapsed or refractory pediatric low-grade glioma harboring a BRAF fusion or rearrangement, or BRAF V600 mutation Recommended Dose 2 380 mg/m administered orally once weekly (not to exceed a dose of 600mg once weekly); OJEMDA can be taken with or without food For full prescribing information, visit dayonebio.com * This indication is approved under accelerated approval based on response rate and duration of response. Continued approval for this indication may be contingent upon verification of clinical benefit in a confirmatory trial. 9 9
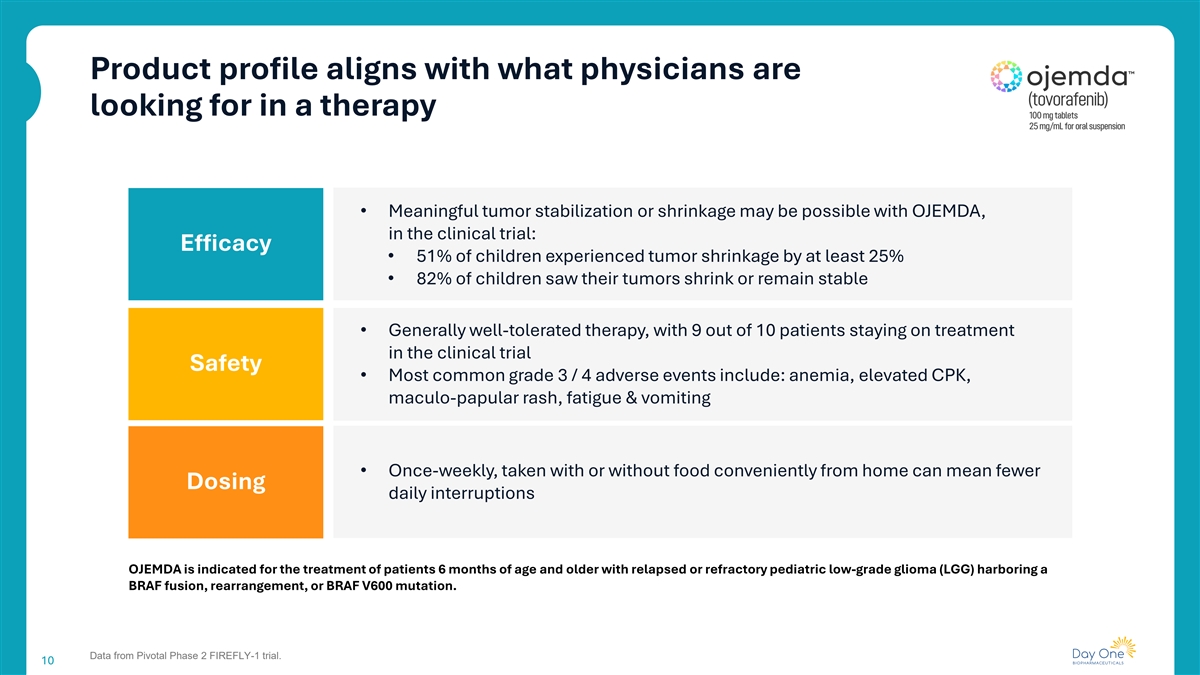
Product profile aligns with what physicians are looking for in a therapy • Meaningful tumor stabilization or shrinkage may be possible with OJEMDA, in the clinical trial: Efficacy • 51% of children experienced tumor shrinkage by at least 25% • 82% of children saw their tumors shrink or remain stable • Generally well-tolerated therapy, with 9 out of 10 patients staying on treatment in the clinical trial Safety • Most common grade 3 / 4 adverse events include: anemia, elevated CPK, maculo-papular rash, fatigue & vomiting • Once-weekly, taken with or without food conveniently from home can mean fewer Dosing daily interruptions OJEMDA is indicated for the treatment of patients 6 months of age and older with relapsed or refractory pediatric low-grade glioma (LGG) harboring a BRAF fusion, rearrangement, or BRAF V600 mutation. Data from Pivotal Phase 2 FIREFLY-1 trial. 10
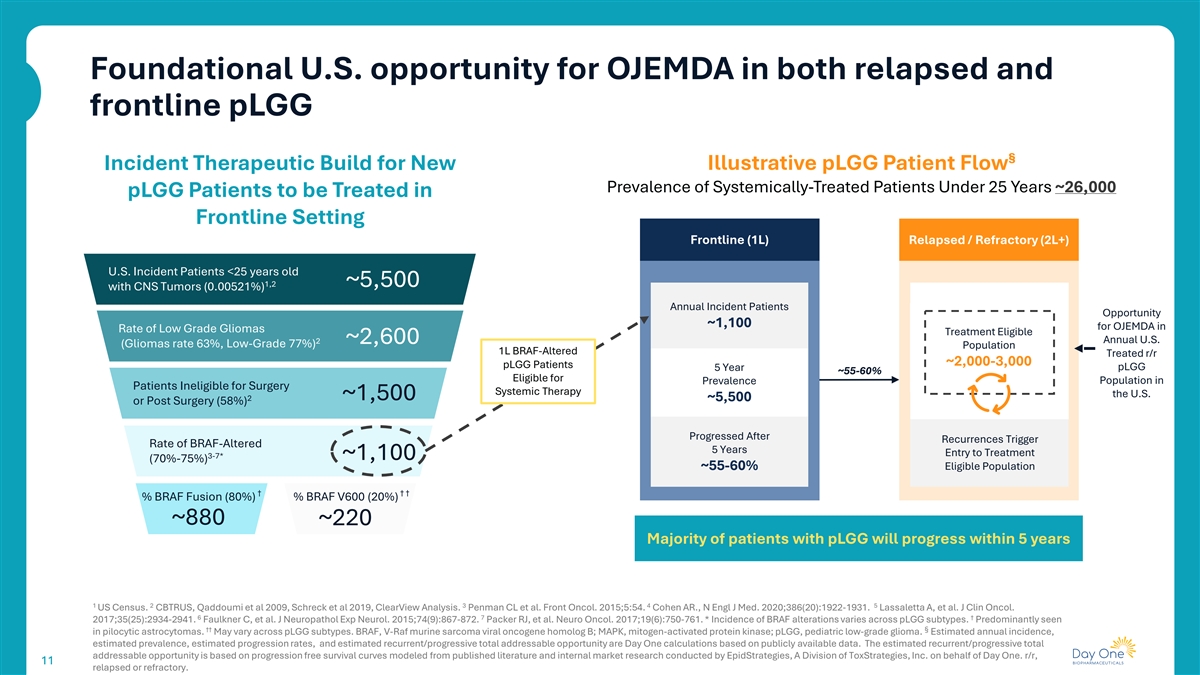
Foundational U.S. opportunity for OJEMDA in both relapsed and frontline pLGG § Incident Therapeutic Build for New Illustrative pLGG Patient Flow Prevalence of Systemically-Treated Patients Under 25 Years ~26,000 pLGG Patients to be Treated in Frontline Setting Frontline (1L) Relapsed / Refractory (2L+) U.S. Incident Patients <25 years old 1,2 ~5,500 with CNS Tumors (0.00521%) Annual Incident Patients Opportunity ~1,100 for OJEMDA in Rate of Low Grade Gliomas Treatment Eligible 2 ~2,600 Annual U.S. (Gliomas rate 63%, Low-Grade 77%) Population 1L BRAF-Altered Treated r/r ~2,000-3,000 pLGG Patients pLGG 5 Year ~55-60% Eligible for Population in Prevalence Patients Ineligible for Surgery Systemic Therapy the U.S. ~1,500 2 ~5,500 or Post Surgery (58%) Progressed After Recurrences Trigger Rate of BRAF-Altered 5 Years Entry to Treatment 3-7* ~1,100 (70%-75%) ~55-60% Eligible Population † † † % BRAF Fusion (80%) % BRAF V600 (20%) ~880 ~220 Majority of patients with pLGG will progress within 5 years 1 2 3 4 5 US Census. CBTRUS, Qaddoumi et al 2009, Schreck et al 2019, ClearView Analysis. Penman CL et al. Front Oncol. 2015;5:54. Cohen AR., N Engl J Med. 2020;386(20):1922-1931. Lassaletta A, et al. J Clin Oncol. 6 7 † 2017;35(25):2934-2941. Faulkner C, et al. J Neuropathol Exp Neurol. 2015;74(9):867-872. Packer RJ, et al. Neuro Oncol. 2017;19(6):750-761. * Incidence of BRAF alterations varies across pLGG subtypes. Predominantly seen †† § in pilocytic astrocytomas. May vary across pLGG subtypes. BRAF, V-Raf murine sarcoma viral oncogene homolog B; MAPK, mitogen-activated protein kinase; pLGG, pediatric low-grade glioma. Estimated annual incidence, estimated prevalence, estimated progression rates, and estimated recurrent/progressive total addressable opportunity are Day One calculations based on publicly available data. The estimated recurrent/progressive total addressable opportunity is based on progression free survival curves modeled from published literature and internal market research conducted by EpidStrategies, A Division of ToxStrategies, Inc. on behalf of Day One. r/r, 11 11 relapsed or refractory.
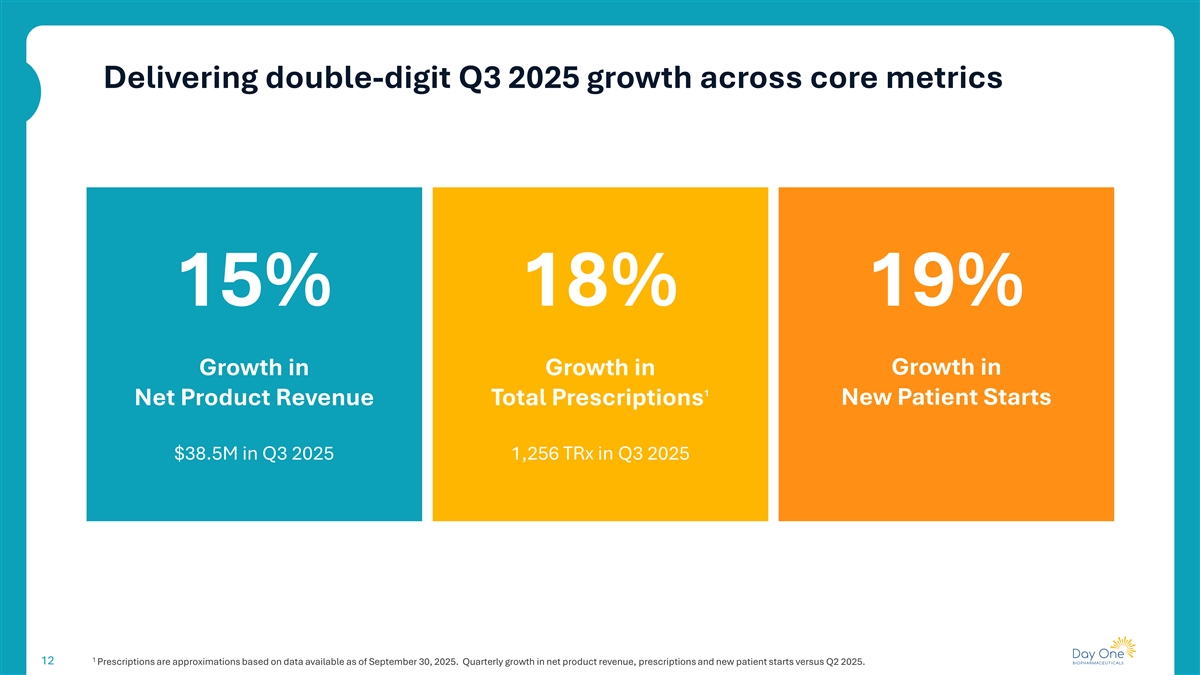
Delivering double-digit Q3 2025 growth across core metrics 15% 18% 19% Growth in Growth in Growth in 1 Net Product Revenue Total Prescriptions New Patient Starts $38.5M in Q3 2025 1,256 TRx in Q3 2025 1 12 Prescriptions are approximations based on data available as of September 30, 2025. Quarterly growth in net product revenue, prescriptions and new patient starts versus Q2 2025.
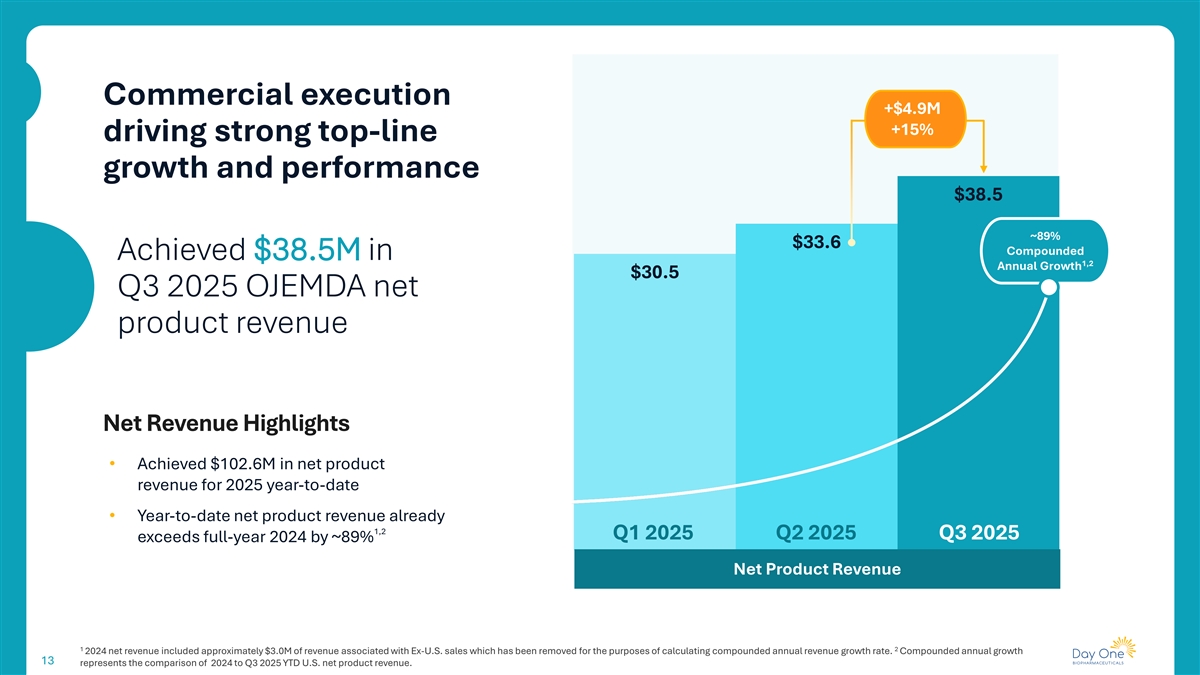
Commercial execution +$4.9M +15% driving strong top-line growth and performance $38.5 ~89% $33.6 Compounded Achieved $38.5M in 1,2 Annual Growth $30.5 Q3 2025 OJEMDA net product revenue Net Revenue Highlights • Achieved $102.6M in net product revenue for 2025 year-to-date • Year-to-date net product revenue already 1,2 Q1 2025 Q2 2025 Q3 2025 exceeds full-year 2024 by ~89% Net Product Revenue 1 2 2024 net revenue included approximately $3.0M of revenue associated with Ex-U.S. sales which has been removed for the purposes of calculating compounded annual revenue growth rate. Compounded annual growth 13 represents the comparison of 2024 to Q3 2025 YTD U.S. net product revenue.
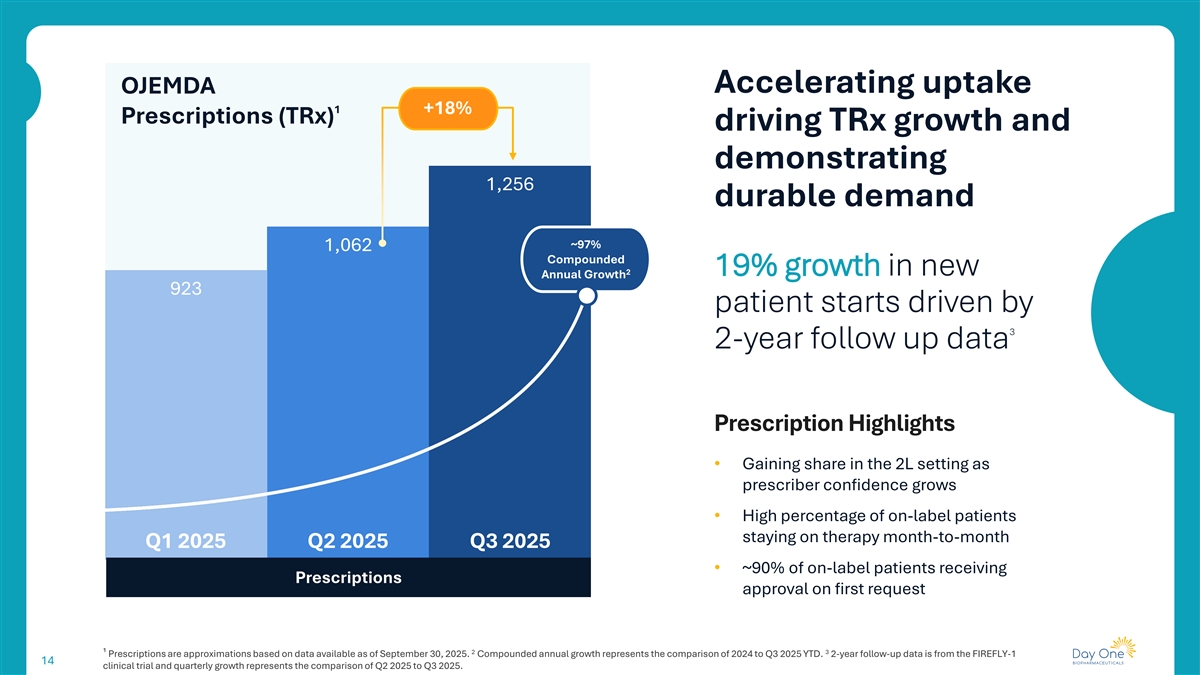
Accelerating uptake OJEMDA 1 +18% Prescriptions (TRx) driving TRx growth and demonstrating 1,256 durable demand ~97% 1,062 Compounded 2 19% growth in new Annual Growth 923 patient starts driven by 3 2-year follow up data Prescription Highlights • Gaining share in the 2L setting as prescriber confidence grows • High percentage of on-label patients staying on therapy month-to-month Q1 2025 Q2 2025 Q3 2025 • ~90% of on-label patients receiving Prescriptions approval on first request 2 3 ¹ Prescriptions are approximations based on data available as of September 30, 2025. Compounded annual growth represents the comparison of 2024 to Q3 2025 YTD. 2-year follow-up data is from the FIREFLY-1 14 clinical trial and quarterly growth represents the comparison of Q2 2025 to Q3 2025.
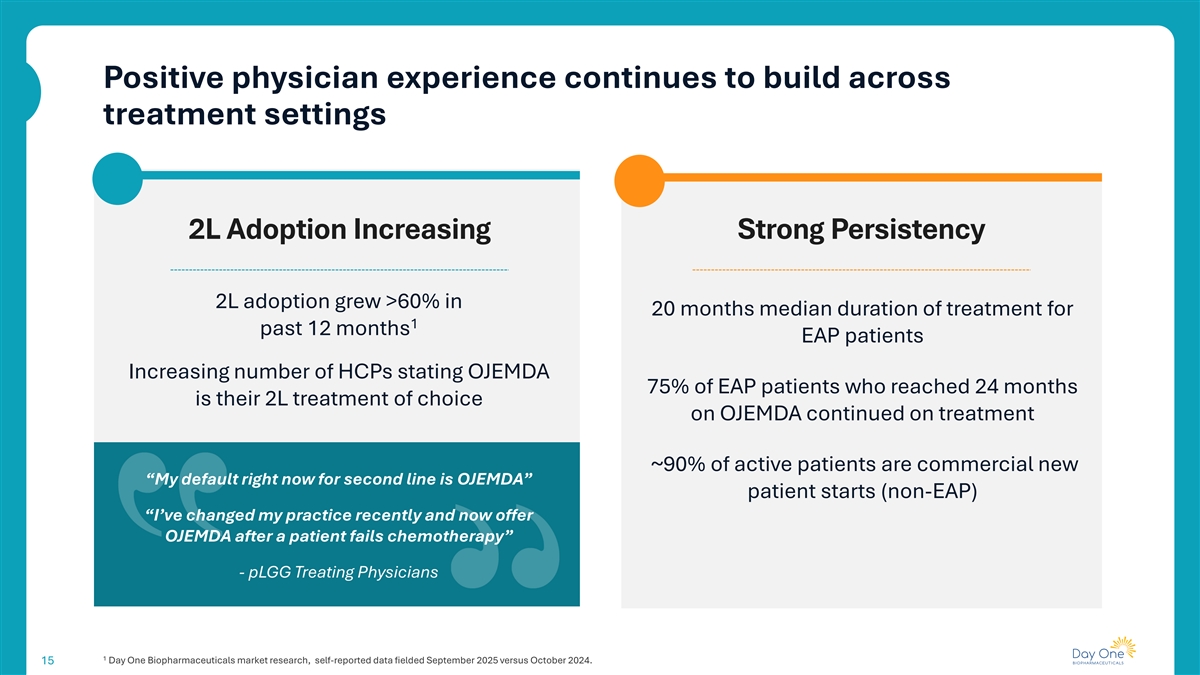
Positive physician experience continues to build across treatment settings 2L Adoption Increasing Strong Persistency 2L adoption grew >60% in 20 months median duration of treatment for 1 past 12 months EAP patients Increasing number of HCPs stating OJEMDA 75% of EAP patients who reached 24 months is their 2L treatment of choice on OJEMDA continued on treatment ~90% of active patients are commercial new “My default right now for second line is OJEMDA” patient starts (non-EAP) “I’ve changed my practice recently and now offer OJEMDA after a patient fails chemotherapy” - pLGG Treating Physicians 1 Day One Biopharmaceuticals market research, self-reported data fielded September 2025 versus October 2024. 15
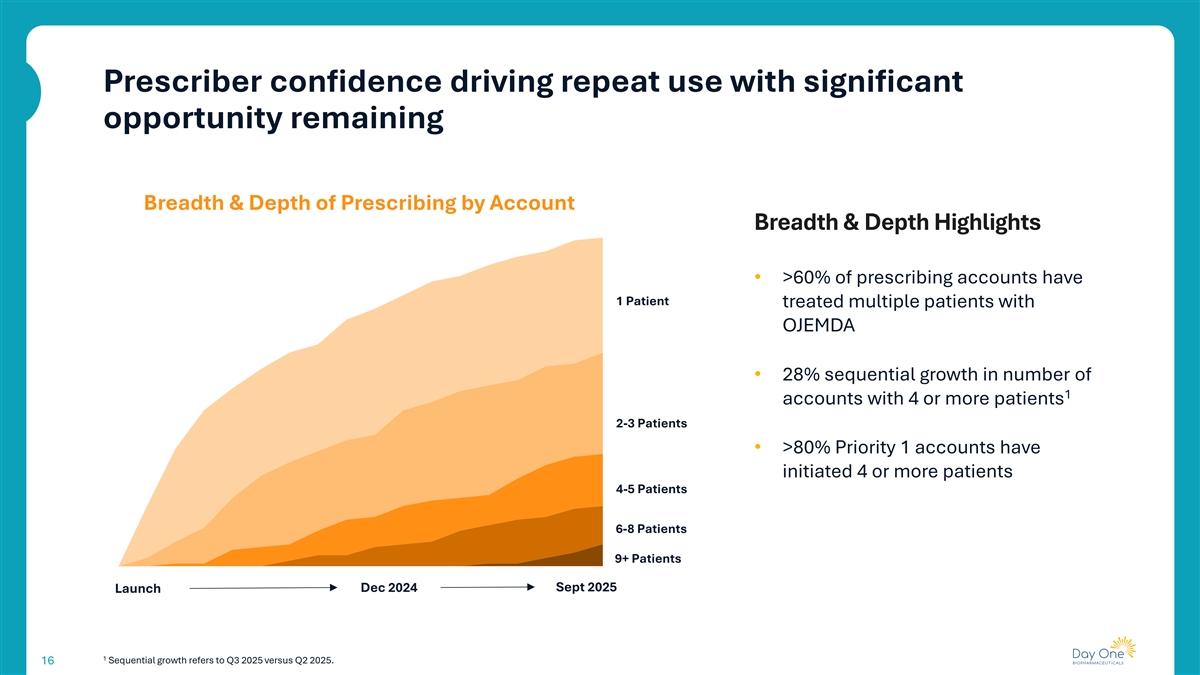
Prescriber confidence driving repeat use with significant opportunity remaining Breadth & Depth of Prescribing by Account Breadth & Depth Highlights • >60% of prescribing accounts have 1 Patient treated multiple patients with OJEMDA • 28% sequential growth in number of 1 accounts with 4 or more patients 2-3 Patients • >80% Priority 1 accounts have initiated 4 or more patients 4-5 Patients 6-8 Patients 9+ Patients Sept 2025 Launch Dec 2024 1 Sequential growth refers to Q3 2025 versus Q2 2025. 16
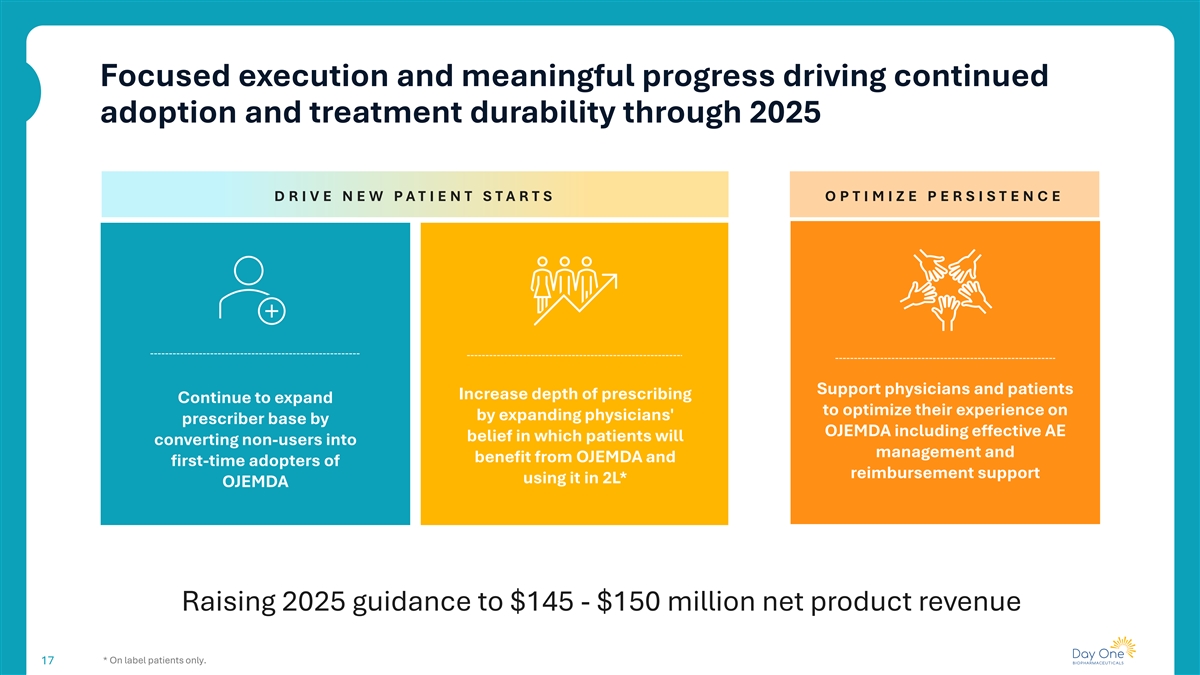
Focused execution and meaningful progress driving continued adoption and treatment durability through 2025 D R I V E NEW PAT I ENT S TA RT S O P T IM IZ E P E RS IS T E N C E Support physicians and patients Increase depth of prescribing Continue to expand to optimize their experience on by expanding physicians' prescriber base by OJEMDA including effective AE belief in which patients will converting non-users into management and benefit from OJEMDA and first-time adopters of reimbursement support using it in 2L* OJEMDA Raising 2025 guidance to $145 - $150 million net product revenue * On label patients only. 17
We continue to strengthen the OJEMDA story through enhancing the target product profile and data generation FIREFLY-1 3-Year Data Highlighting clinical stability following Establishing treatment with OJEMDA and opportunity for OJEMDA as the retreatment Standard of Care in 2L r/r BRAF- Potential to further expand physician altered pLGG confidence and adoption while reinforcing target product profile Presentation at SNO conference in November 2025 and publication efforts underway 18
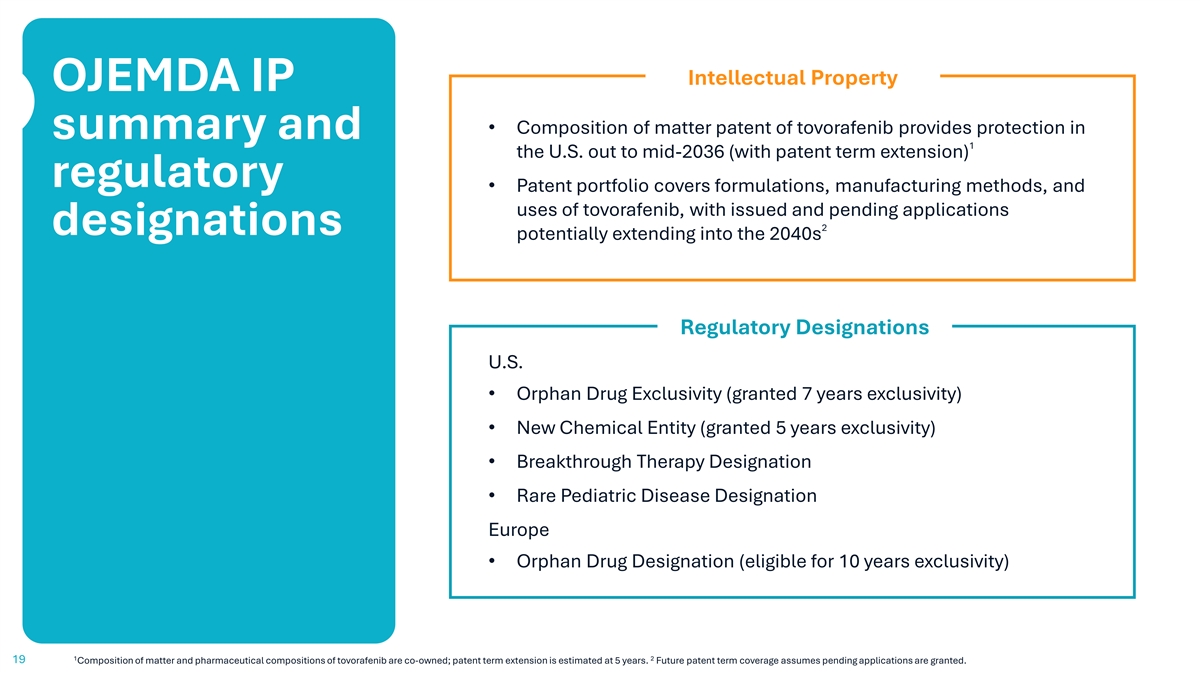
Intellectual Property OJEMDA IP • Composition of matter patent of tovorafenib provides protection in summary and 1 the U.S. out to mid-2036 (with patent term extension) regulatory • Patent portfolio covers formulations, manufacturing methods, and uses of tovorafenib, with issued and pending applications 2 designations potentially extending into the 2040s Regulatory Designations U.S. • Orphan Drug Exclusivity (granted 7 years exclusivity) • New Chemical Entity (granted 5 years exclusivity) • Breakthrough Therapy Designation • Rare Pediatric Disease Designation Europe • Orphan Drug Designation (eligible for 10 years exclusivity) 1 2 19 Composition of matter and pharmaceutical compositions of tovorafenib are co-owned; patent term extension is estimated at 5 years. Future patent term coverage assumes pending applications are granted.
3-year follow- up data from the FIREFLY-1 trial studying OJEMDA Phase 2 FIREFLY-1 Trial 20
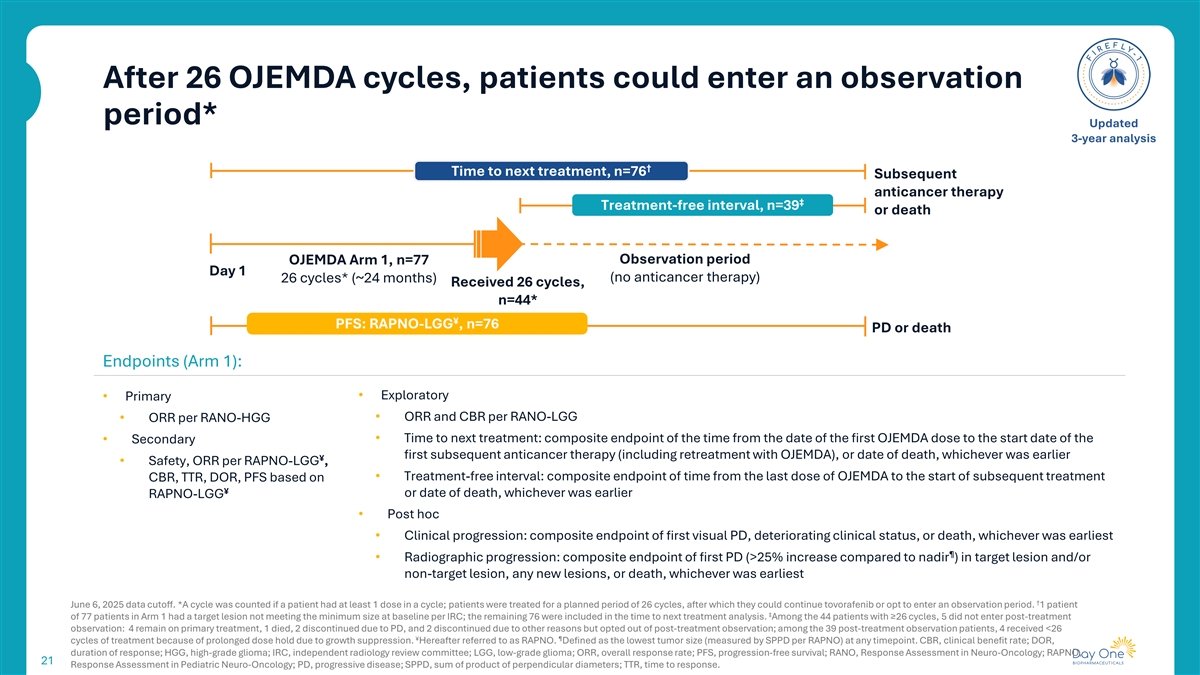
After 26 OJEMDA cycles, patients could enter an observation period* Updated 3-year analysis † Time to next treatment, n=76 Subsequent anticancer therapy ‡ Treatment-free interval, n=39 or death Observation period OJEMDA Arm 1, n=77 Day 1 (no anticancer therapy) 26 cycles* (~24 months) Received 26 cycles, n=44* ¥ PFS: RAPNO-LGG , n=76 PD or death Endpoints (Arm 1): • Exploratory • Primary • ORR and CBR per RANO-LGG • ORR per RANO-HGG • Time to next treatment: composite endpoint of the time from the date of the first OJEMDA dose to the start date of the • Secondary first subsequent anticancer therapy (including retreatment with OJEMDA), or date of death, whichever was earlier ¥ • Safety, ORR per RAPNO-LGG , • Treatment-free interval: composite endpoint of time from the last dose of OJEMDA to the start of subsequent treatment CBR, TTR, DOR, PFS based on ¥ or date of death, whichever was earlier RAPNO-LGG • Post hoc • Clinical progression: composite endpoint of first visual PD, deteriorating clinical status, or death, whichever was earliest ¶ • Radiographic progression: composite endpoint of first PD (>25% increase compared to nadir ) in target lesion and/or non-target lesion, any new lesions, or death, whichever was earliest † June 6, 2025 data cutoff. *A cycle was counted if a patient had at least 1 dose in a cycle; patients were treated for a planned period of 26 cycles, after which they could continue tovorafenib or opt to enter an observation period. 1 patient ‡ of 77 patients in Arm 1 had a target lesion not meeting the minimum size at baseline per IRC; the remaining 76 were included in the time to next treatment analysis. Among the 44 patients with ≥26 cycles, 5 did not enter post-treatment observation: 4 remain on primary treatment, 1 died, 2 discontinued due to PD, and 2 discontinued due to other reasons but opted out of post-treatment observation; among the 39 post-treatment observation patients, 4 received <26 ¥ ¶ cycles of treatment because of prolonged dose hold due to growth suppression. Hereafter referred to as RAPNO. Defined as the lowest tumor size (measured by SPPD per RAPNO) at any timepoint. CBR, clinical benefit rate; DOR, duration of response; HGG, high-grade glioma; IRC, independent radiology review committee; LGG, low-grade glioma; ORR, overall response rate; PFS, progression-free survival; RANO, Response Assessment in Neuro-Oncology; RAPNO, 21 Response Assessment in Pediatric Neuro-Oncology; PD, progressive disease; SPPD, sum of product of perpendicular diameters; TTR, time to response.
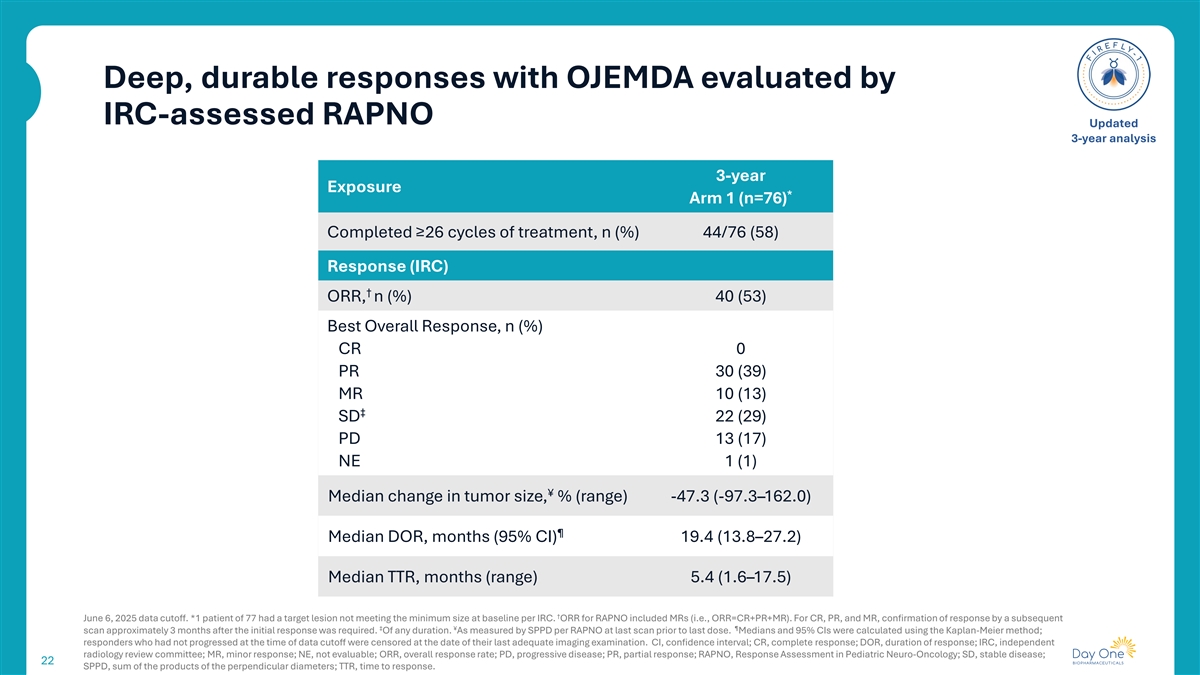
Deep, durable responses with OJEMDA evaluated by IRC-assessed RAPNO Updated 3-year analysis 3-year Exposure * Arm 1 (n=76) Completed ≥26 cycles of treatment, n (%) 44/76 (58) Response (IRC) † ORR, n (%) 40 (53) Best Overall Response, n (%) CR 0 PR 30 (39) MR 10 (13) ‡ SD 22 (29) PD 13 (17) NE 1 (1) ¥ Median change in tumor size, % (range) -47.3 (-97.3–162.0) ¶ Median DOR, months (95% CI) 19.4 (13.8–27.2) Median TTR, months (range) 5.4 (1.6–17.5) † June 6, 2025 data cutoff. *1 patient of 77 had a target lesion not meeting the minimum size at baseline per IRC. ORR for RAPNO included MRs (i.e., ORR=CR+PR+MR). For CR, PR, and MR, confirmation of response by a subsequent ‡ ¥ ¶ scan approximately 3 months after the initial response was required. Of any duration. As measured by SPPD per RAPNO at last scan prior to last dose. Medians and 95% CIs were calculated using the Kaplan-Meier method; responders who had not progressed at the time of data cutoff were censored at the date of their last adequate imaging examination. CI, confidence interval; CR, complete response; DOR, duration of response; IRC, independent radiology review committee; MR, minor response; NE, not evaluable; ORR, overall response rate; PD, progressive disease; PR, partial response; RAPNO, Response Assessment in Pediatric Neuro-Oncology; SD, stable disease; 22 SPPD, sum of the products of the perpendicular diameters; TTR, time to response.
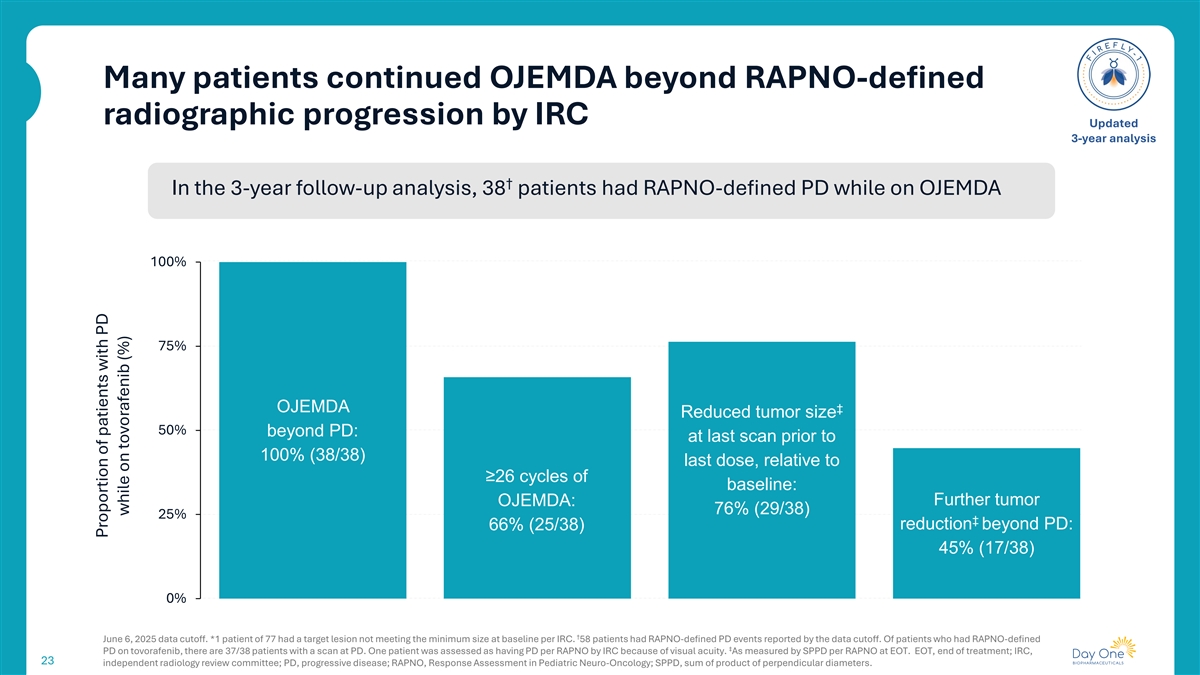
Many patients continued OJEMDA beyond RAPNO-defined radiographic progression by IRC Updated 3-year analysis † In the 3-year follow-up analysis, 38 patients had RAPNO-defined PD while on OJEMDA 100% 75% OJEMDA ‡ Reduced tumor size 50% beyond PD: at last scan prior to 100% (38/38) last dose, relative to ≥26 cycles of baseline: Further tumor OJEMDA: 76% (29/38) 25% ‡ 66% (25/38) reduction beyond PD: 45% (17/38) 0% † June 6, 2025 data cutoff. *1 patient of 77 had a target lesion not meeting the minimum size at baseline per IRC. 58 patients had RAPNO-defined PD events reported by the data cutoff. Of patients who had RAPNO-defined ‡ PD on tovorafenib, there are 37/38 patients with a scan at PD. One patient was assessed as having PD per RAPNO by IRC because of visual acuity. As measured by SPPD per RAPNO at EOT. EOT, end of treatment; IRC, 23 independent radiology review committee; PD, progressive disease; RAPNO, Response Assessment in Pediatric Neuro-Oncology; SPPD, sum of product of perpendicular diameters. Proportion of patients with PD while on tovorafenib (%)
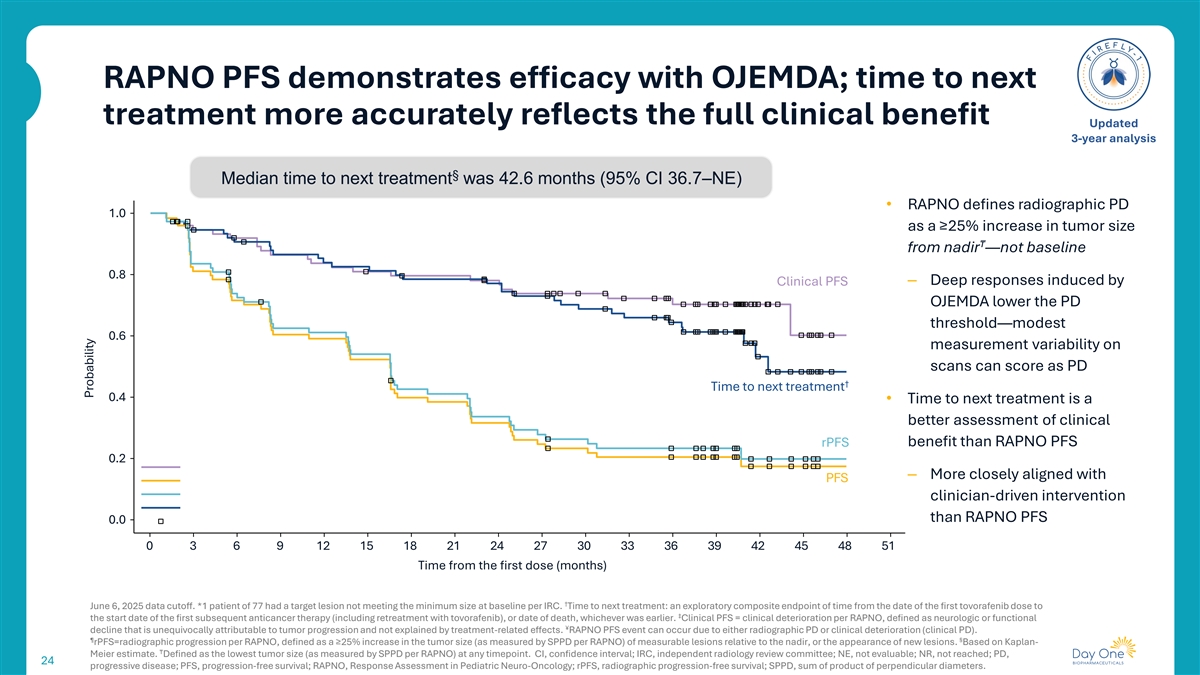
RAPNO PFS demonstrates efficacy with OJEMDA; time to next treatment more accurately reflects the full clinical benefit Updated 3-year analysis § Median time to next treatment was 42.6 months (95% CI 36.7–NE) • RAPNO defines radiographic PD 1.0 as a ≥25% increase in tumor size ₸ from nadir —not baseline 0.8 – Deep responses induced by Clinical PFS OJEMDA lower the PD threshold—modest 0.6 measurement variability on scans can score as PD † Time to next treatment 0.4 • Time to next treatment is a better assessment of clinical benefit than RAPNO PFS rPFS 0.2 – More closely aligned with PFS clinician-driven intervention than RAPNO PFS 0.0 0 3 6 9 12 15 18 21 24 27 30 33 36 39 42 45 48 51 Time from the first dose (months) † June 6, 2025 data cutoff. *1 patient of 77 had a target lesion not meeting the minimum size at baseline per IRC. Time to next treatment: an exploratory composite endpoint of time from the date of the first tovorafenib dose to ‡ the start date of the first subsequent anticancer therapy (including retreatment with tovorafenib), or date of death, whichever was earlier. Clinical PFS = clinical deterioration per RAPNO, defined as neurologic or functional ¥ decline that is unequivocally attributable to tumor progression and not explained by treatment-related effects. RAPNO PFS event can occur due to either radiographic PD or clinical deterioration (clinical PD). ¶ § rPFS=radiographic progression per RAPNO, defined as a ≥25% increase in the tumor size (as measured by SPPD per RAPNO) of measurable lesions relative to the nadir, or the appearance of new lesions. Based on Kaplan- ₸ Meier estimate. Defined as the lowest tumor size (as measured by SPPD per RAPNO) at any timepoint. CI, confidence interval; IRC, independent radiology review committee; NE, not evaluable; NR, not reached; PD, 24 progressive disease; PFS, progression-free survival; RAPNO, Response Assessment in Pediatric Neuro-Oncology; rPFS, radiographic progression-free survival; SPPD, sum of product of perpendicular diameters. Probability
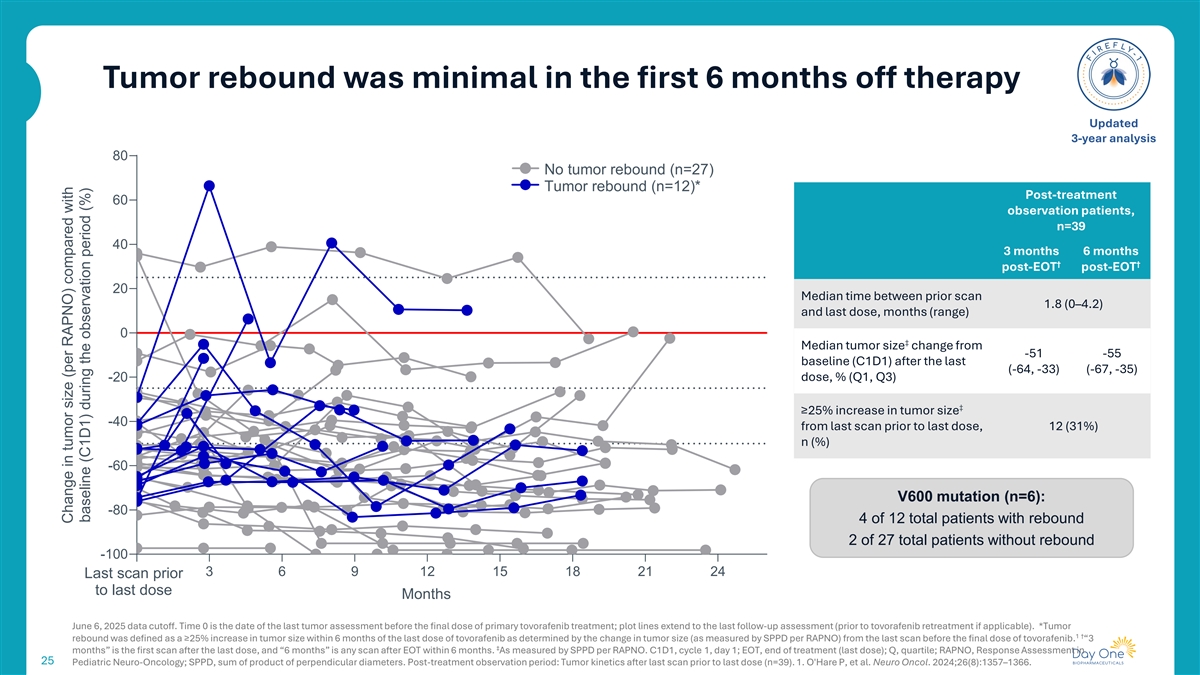
Tumor rebound was minimal in the first 6 months off therapy Updated 3-year analysis 80 No tumor rebound (n=27) Tumor rebound (n=12)* Post-treatment 60 observation patients, n=39 40 3 months 6 months † † post-EOT post-EOT 20 Median time between prior scan 1.8 (0–4.2) and last dose, months (range) 0 ‡ Median tumor size change from -51 -55 baseline (C1D1) after the last (-64, -33) (-67, -35) -20 dose, % (Q1, Q3) ‡ ≥25% increase in tumor size -40 from last scan prior to last dose, 12 (31%) n (%) -60 V600 mutation (n=6): -80 4 of 12 total patients with rebound 2 of 27 total patients without rebound -100 0 3 6 9 12 15 18 21 24 Last scan prior to last dose Months June 6, 2025 data cutoff. Time 0 is the date of the last tumor assessment before the final dose of primary tovorafenib treatment; plot lines extend to the last follow-up assessment (prior to tovorafenib retreatment if applicable). *Tumor 1 † rebound was defined as a ≥25% increase in tumor size within 6 months of the last dose of tovorafenib as determined by the change in tumor size (as measured by SPPD per RAPNO) from the last scan before the final dose of tovorafenib. “3 ‡ months” is the first scan after the last dose, and “6 months” is any scan after EOT within 6 months. As measured by SPPD per RAPNO. C1D1, cycle 1, day 1; EOT, end of treatment (last dose); Q, quartile; RAPNO, Response Assessment in 25 Pediatric Neuro-Oncology; SPPD, sum of product of perpendicular diameters. Post-treatment observation period: Tumor kinetics after last scan prior to last dose (n=39). 1. O'Hare P, et al. Neuro Oncol. 2024;26(8):1357–1366. Change in tumor size (per RAPNO) compared with baseline (C1D1) during the observation period (%)
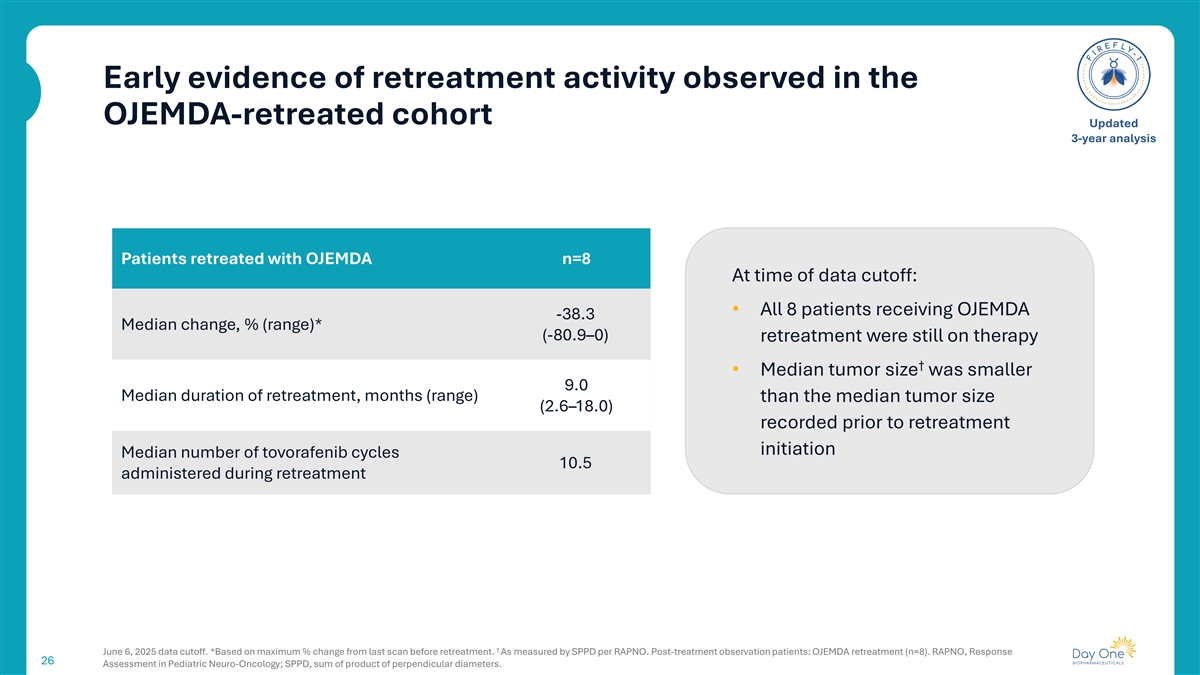
Early evidence of retreatment activity observed in the OJEMDA-retreated cohort Updated 3-year analysis Patients retreated with OJEMDA n=8 At time of data cutoff: • All 8 patients receiving OJEMDA -38.3 Median change, % (range)* (-80.9–0) retreatment were still on therapy † • Median tumor size was smaller 9.0 Median duration of retreatment, months (range) than the median tumor size (2.6–18.0) recorded prior to retreatment initiation Median number of tovorafenib cycles 10.5 administered during retreatment † June 6, 2025 data cutoff. *Based on maximum % change from last scan before retreatment. As measured by SPPD per RAPNO. Post-treatment observation patients: OJEMDA retreatment (n=8). RAPNO, Response 26 Assessment in Pediatric Neuro-Oncology; SPPD, sum of product of perpendicular diameters.
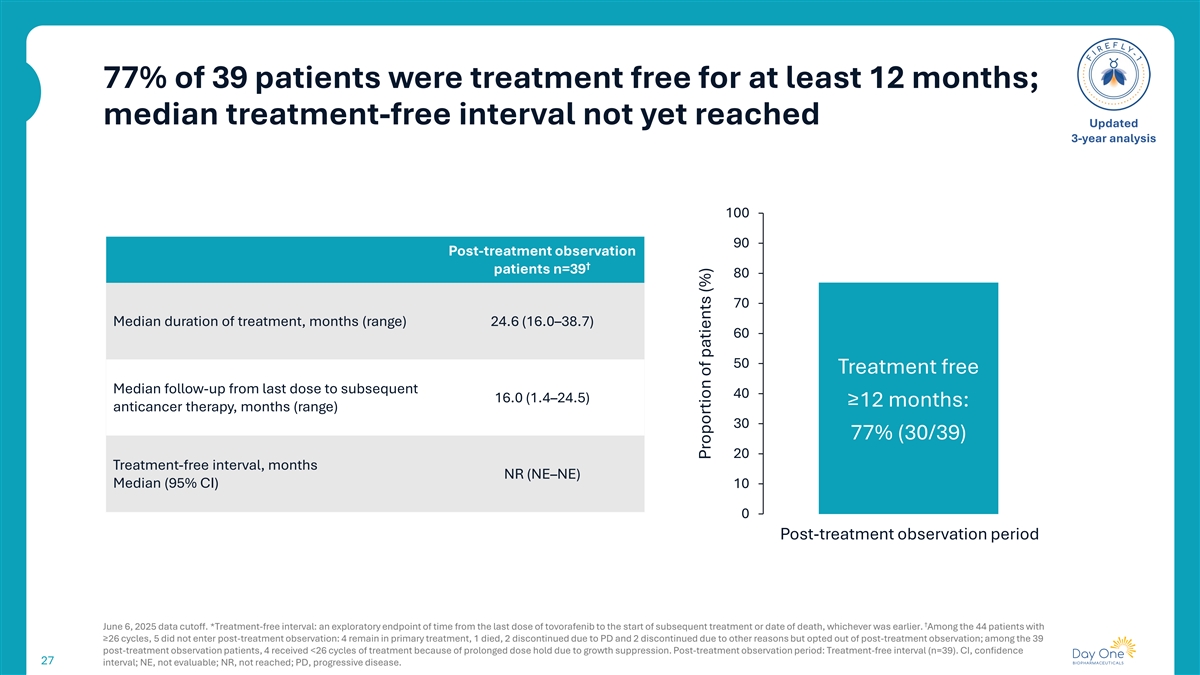
77% of 39 patients were treatment free for at least 12 months; median treatment-free interval not yet reached Updated 3-year analysis 100 90 Post-treatment observation † patients n=39 80 70 Median duration of treatment, months (range) 24.6 (16.0–38.7) 60 50 Treatment free Median follow-up from last dose to subsequent 40 16.0 (1.4–24.5) ≥12 months: anticancer therapy, months (range) 30 77% (30/39) 20 Treatment-free interval, months NR (NE–NE) Median (95% CI) 10 0 Post-treatment observation period † June 6, 2025 data cutoff. *Treatment-free interval: an exploratory endpoint of time from the last dose of tovorafenib to the start of subsequent treatment or date of death, whichever was earlier. Among the 44 patients with ≥26 cycles, 5 did not enter post-treatment observation: 4 remain in primary treatment, 1 died, 2 discontinued due to PD and 2 discontinued due to other reasons but opted out of post-treatment observation; among the 39 post-treatment observation patients, 4 received <26 cycles of treatment because of prolonged dose hold due to growth suppression. Post-treatment observation period: Treatment-free interval (n=39). CI, confidence 27 interval; NE, not evaluable; NR, not reached; PD, progressive disease. Proportion of patients (%)
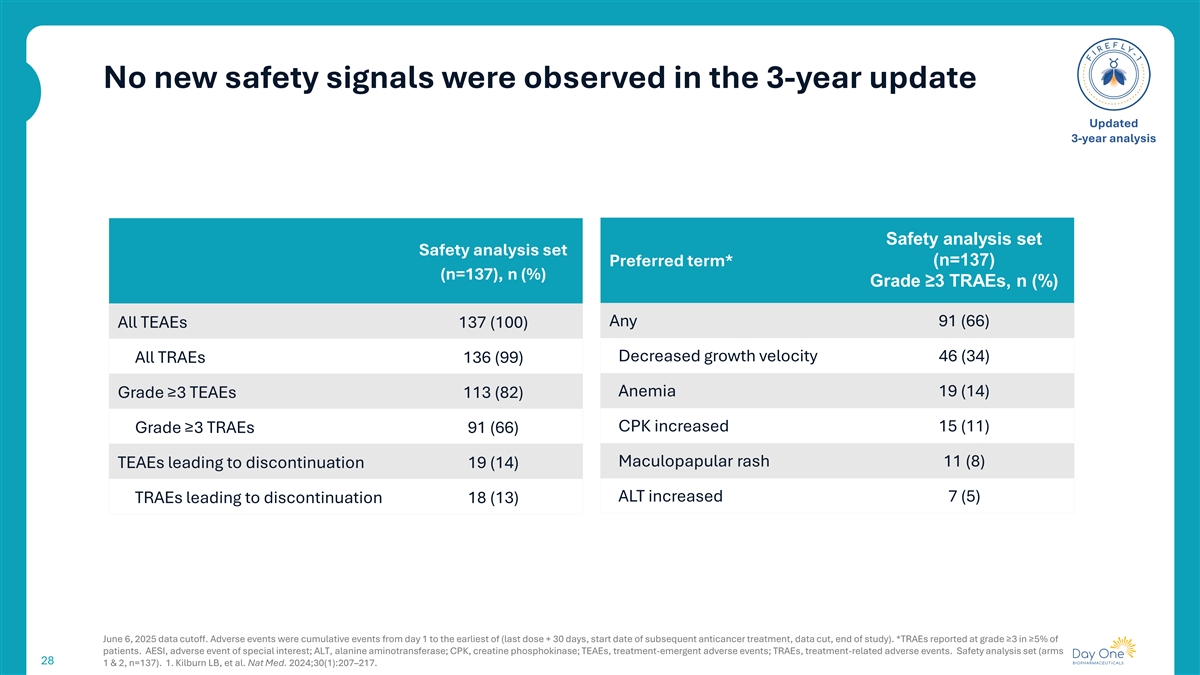
No new safety signals were observed in the 3-year update Updated 3-year analysis Safety analysis set Safety analysis set Preferred term* (n=137) (n=137), n (%) Grade ≥3 TRAEs, n (%) Any 91 (66) All TEAEs 137 (100) Decreased growth velocity 46 (34) All TRAEs 136 (99) Anemia 19 (14) Grade ≥3 TEAEs 113 (82) CPK increased 15 (11) Grade ≥3 TRAEs 91 (66) Maculopapular rash 11 (8) TEAEs leading to discontinuation 19 (14) ALT increased 7 (5) TRAEs leading to discontinuation 18 (13) June 6, 2025 data cutoff. Adverse events were cumulative events from day 1 to the earliest of (last dose + 30 days, start date of subsequent anticancer treatment, data cut, end of study). *TRAEs reported at grade ≥3 in ≥5% of patients. AESI, adverse event of special interest; ALT, alanine aminotransferase; CPK, creatine phosphokinase; TEAEs, treatment-emergent adverse events; TRAEs, treatment-related adverse events. Safety analysis set (arms 28 1 & 2, n=137). 1. Kilburn LB, et al. Nat Med. 2024;30(1):207–217.

FIREFLY-2 Pivotal Phase 3 trial of tovorafenib in front-line pLGG Bradon Living with pLGG since age 11 29
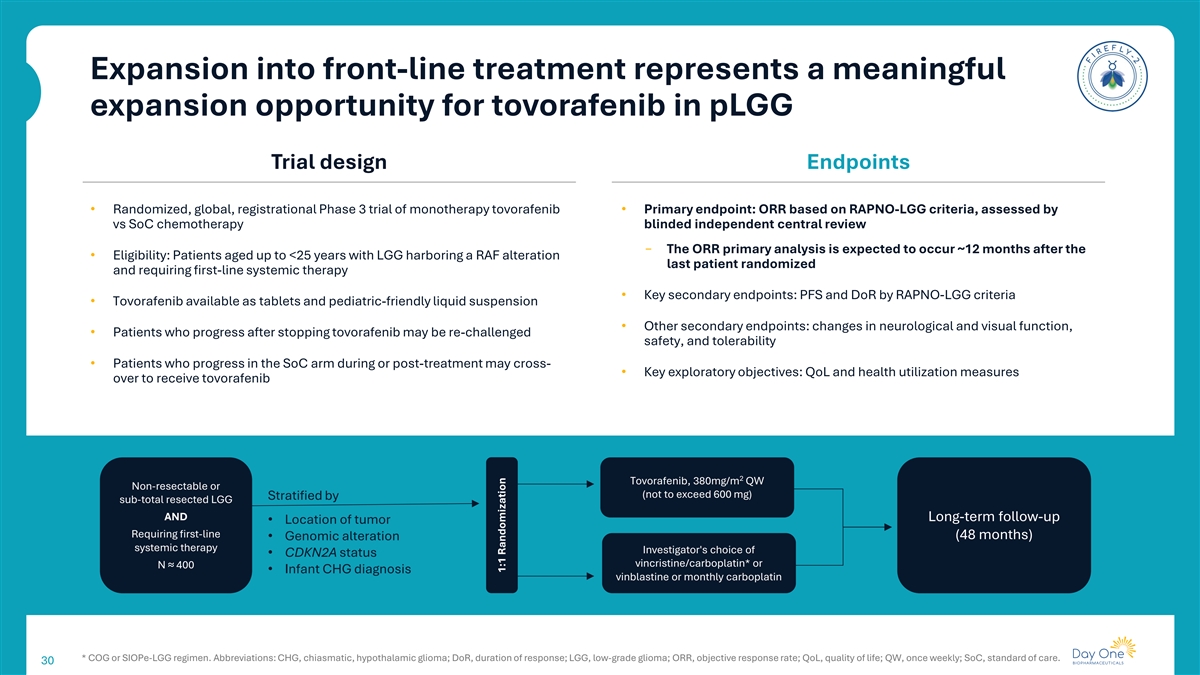
Expansion into front-line treatment represents a meaningful expansion opportunity for tovorafenib in pLGG Trial design Endpoints • Randomized, global, registrational Phase 3 trial of monotherapy tovorafenib • Primary endpoint: ORR based on RAPNO-LGG criteria, assessed by vs SoC chemotherapy blinded independent central review ‒ The ORR primary analysis is expected to occur ~12 months after the • Eligibility: Patients aged up to <25 years with LGG harboring a RAF alteration last patient randomized and requiring first-line systemic therapy • Key secondary endpoints: PFS and DoR by RAPNO-LGG criteria • Tovorafenib available as tablets and pediatric-friendly liquid suspension • Other secondary endpoints: changes in neurological and visual function, • Patients who progress after stopping tovorafenib may be re-challenged safety, and tolerability • Patients who progress in the SoC arm during or post-treatment may cross- • Key exploratory objectives: QoL and health utilization measures over to receive tovorafenib 2 Tovorafenib, 380mg/m QW Non-resectable or (not to exceed 600 mg) Stratified by sub-total resected LGG AND Long-term follow-up • Location of tumor Requiring first-line • Genomic alteration (48 months) systemic therapy Investigator's choice of • CDKN2A status vincristine/carboplatin* or N ≈ 400 • Infant CHG diagnosis vinblastine or monthly carboplatin * COG or SIOPe-LGG regimen. Abbreviations: CHG, chiasmatic, hypothalamic glioma; DoR, duration of response; LGG, low-grade glioma; ORR, objective response rate; QoL, quality of life; QW, once weekly; SoC, standard of care. 30 1:1 Randomization

Emi-Le B7-H4-targeted antibody-drug conjugate (ADC) 31
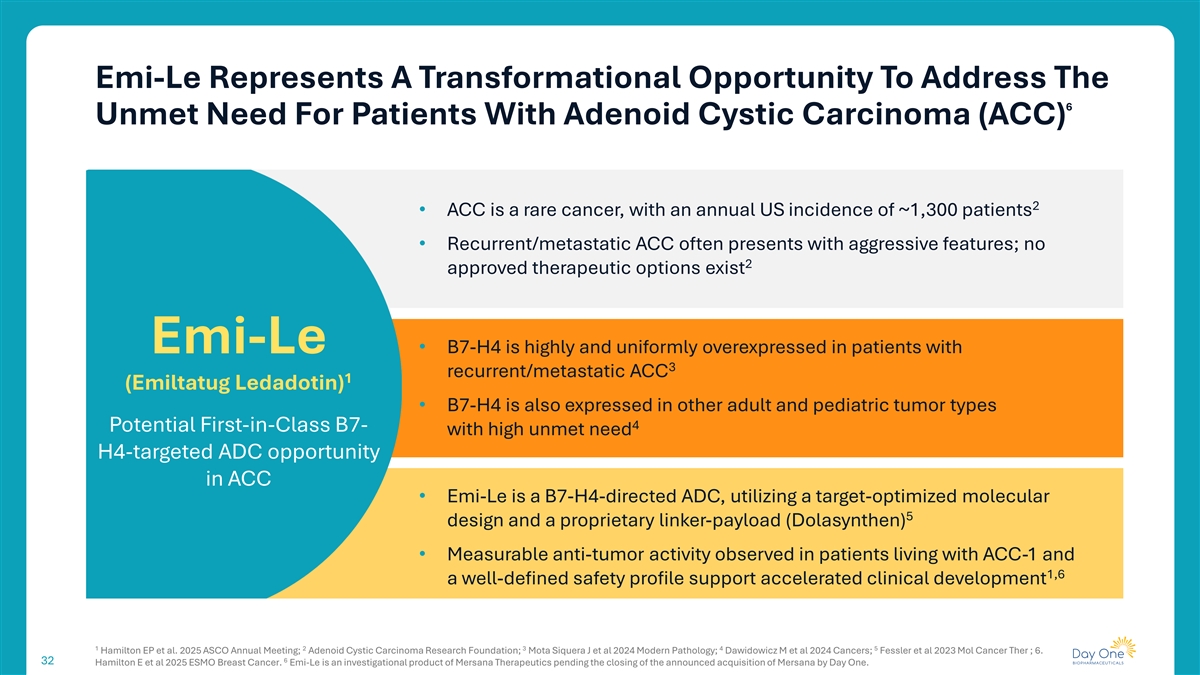
Emi-Le Represents A Transformational Opportunity To Address The 6 Unmet Need For Patients With Adenoid Cystic Carcinoma (ACC) 2 • ACC is a rare cancer, with an annual US incidence of ~1,300 patients • Recurrent/metastatic ACC often presents with aggressive features; no 2 approved therapeutic options exist Emi-Le • B7-H4 is highly and uniformly overexpressed in patients with 3 recurrent/metastatic ACC 1 (Emiltatug Ledadotin) • B7-H4 is also expressed in other adult and pediatric tumor types 4 Potential First-in-Class B7- with high unmet need H4-targeted ADC opportunity in ACC • Emi-Le is a B7-H4-directed ADC, utilizing a target-optimized molecular 5 design and a proprietary linker-payload (Dolasynthen) • Measurable anti-tumor activity observed in patients living with ACC-1 and 1,6 a well-defined safety profile support accelerated clinical development 1 2 3 4 5 Hamilton EP et al. 2025 ASCO Annual Meeting; Adenoid Cystic Carcinoma Research Foundation; Mota Siquera J et al 2024 Modern Pathology; Dawidowicz M et al 2024 Cancers; Fessler et al 2023 Mol Cancer Ther ; 6. 6 32 Hamilton E et al 2025 ESMO Breast Cancer. Emi-Le is an investigational product of Mersana Therapeutics pending the closing of the announced acquisition of Mersana by Day One.

DAY301 PTK7-targeted antibody-drug conjugate (ADC) 33
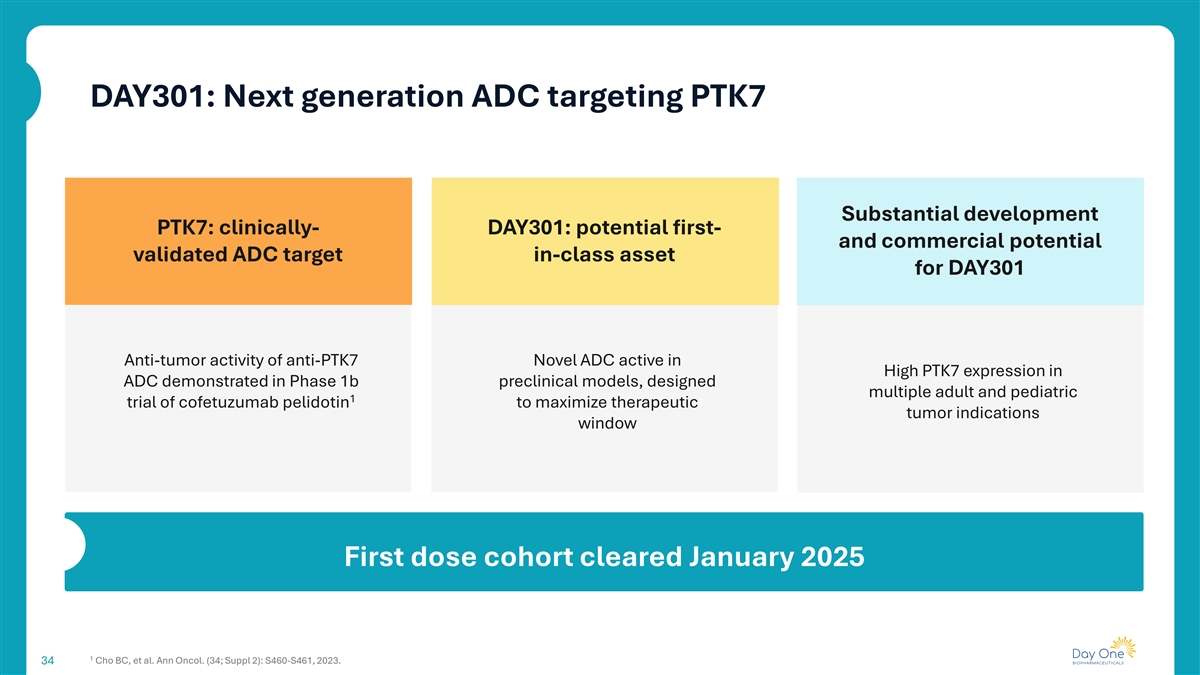
DAY301: Next generation ADC targeting PTK7 Substantial development PTK7: clinically- DAY301: potential first- and commercial potential validated ADC target in-class asset for DAY301 Anti-tumor activity of anti-PTK7 Novel ADC active in High PTK7 expression in ADC demonstrated in Phase 1b preclinical models, designed multiple adult and pediatric 1 trial of cofetuzumab pelidotin to maximize therapeutic tumor indications window First dose cohort cleared January 2025 1 Cho BC, et al. Ann Oncol. (34; Suppl 2): S460-S461, 2023. 34
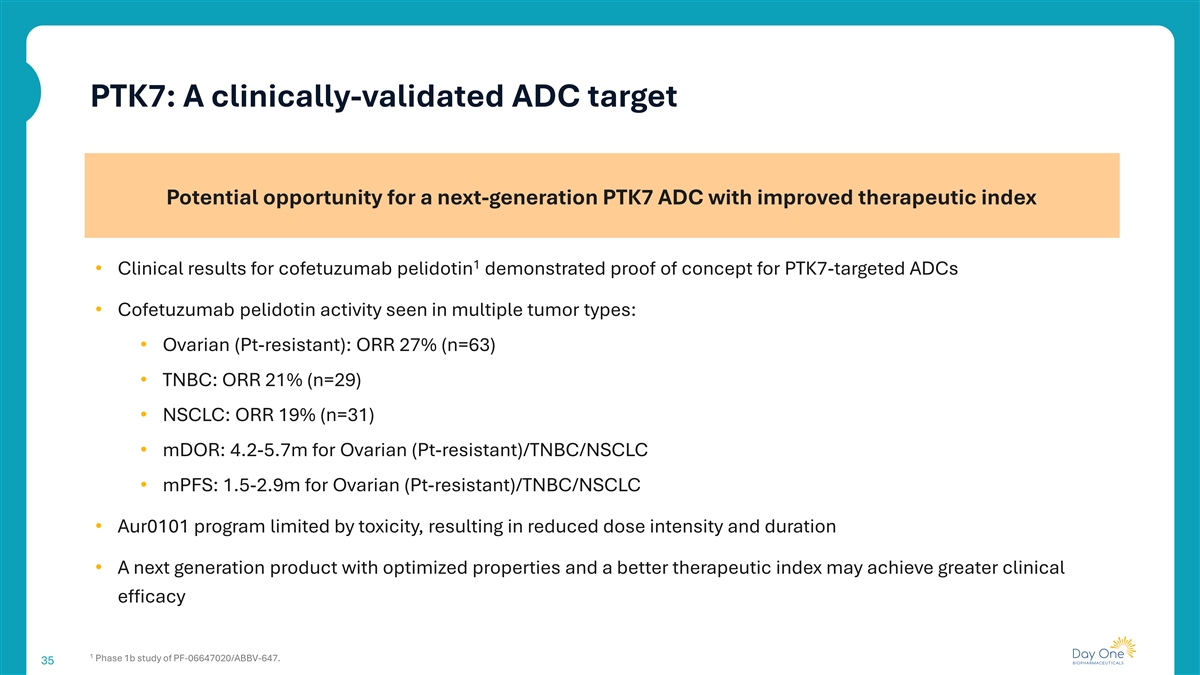
PTK7: A clinically-validated ADC target Potential opportunity for a next-generation PTK7 ADC with improved therapeutic index 1 • Clinical results for cofetuzumab pelidotin demonstrated proof of concept for PTK7-targeted ADCs • Cofetuzumab pelidotin activity seen in multiple tumor types: • Ovarian (Pt-resistant): ORR 27% (n=63) • TNBC: ORR 21% (n=29) • NSCLC: ORR 19% (n=31) • mDOR: 4.2-5.7m for Ovarian (Pt-resistant)/TNBC/NSCLC • mPFS: 1.5-2.9m for Ovarian (Pt-resistant)/TNBC/NSCLC • Aur0101 program limited by toxicity, resulting in reduced dose intensity and duration • A next generation product with optimized properties and a better therapeutic index may achieve greater clinical efficacy 1 Phase 1b study of PF-06647020/ABBV-647. 35
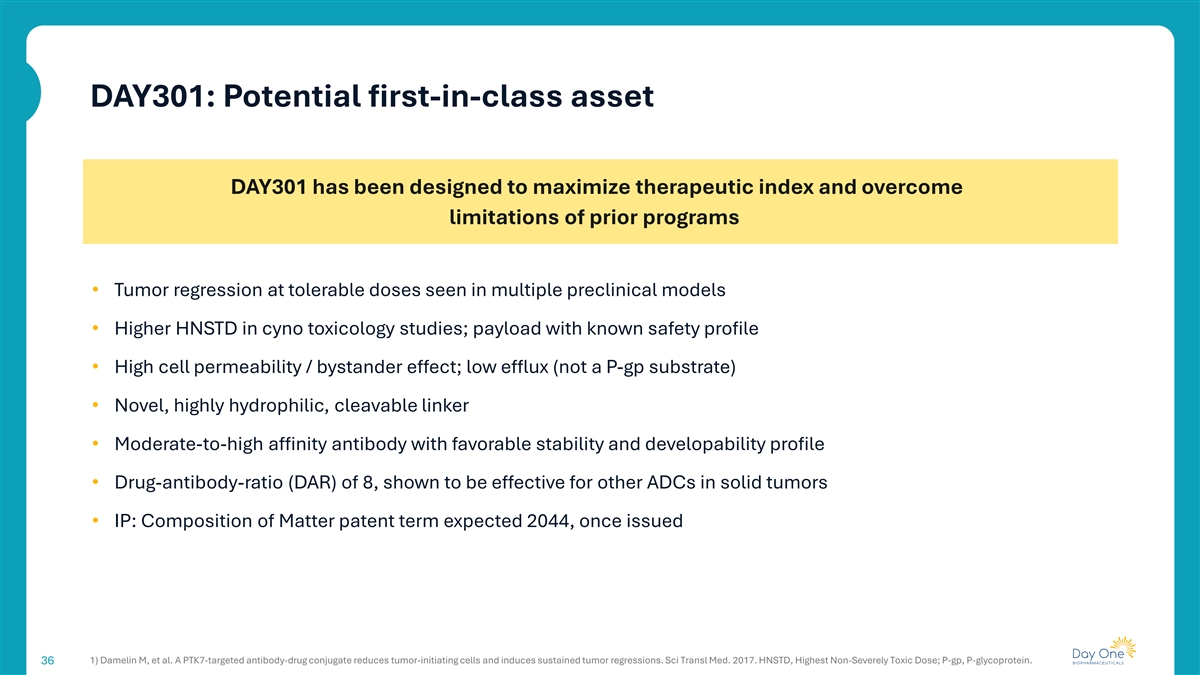
DAY301: Potential first-in-class asset DAY301 has been designed to maximize therapeutic index and overcome limitations of prior programs • Tumor regression at tolerable doses seen in multiple preclinical models • Higher HNSTD in cyno toxicology studies; payload with known safety profile • High cell permeability / bystander effect; low efflux (not a P-gp substrate) • Novel, highly hydrophilic, cleavable linker • Moderate-to-high affinity antibody with favorable stability and developability profile • Drug-antibody-ratio (DAR) of 8, shown to be effective for other ADCs in solid tumors • IP: Composition of Matter patent term expected 2044, once issued 1) Damelin M, et al. A PTK7-targeted antibody-drug conjugate reduces tumor-initiating cells and induces sustained tumor regressions. Sci Transl Med. 2017. HNSTD, Highest Non-Severely Toxic Dose; P-gp, P-glycoprotein. 36
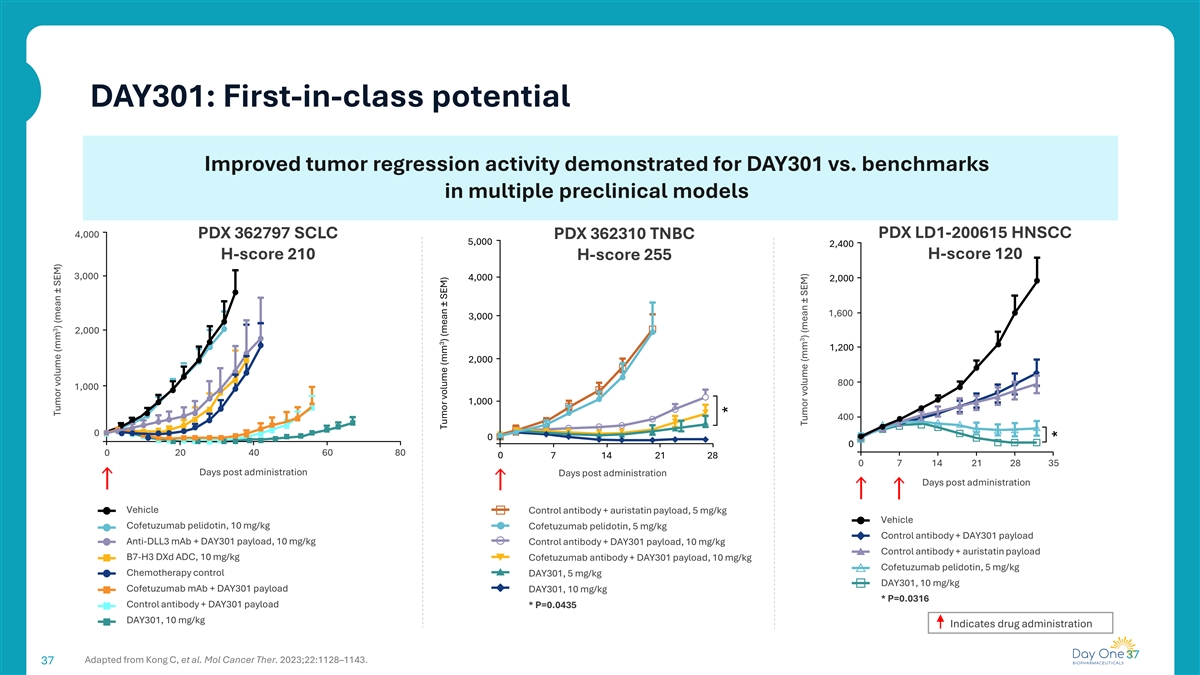
DAY301: First-in-class potential Improved tumor regression activity demonstrated for DAY301 vs. benchmarks in multiple preclinical models 4,000 PDX 362797 SCLC PDX 362310 TNBC PDX LD1-200615 HNSCC 5,000 2,400 H-score 120 H-score 210 H-score 255 3,000 4,000 2,000 1,600 3,000 2,000 1,200 2,000 800 1,000 1,000 400 0 0 0 0 20 40 60 80 0 7 14 21 28 0 7 14 21 28 35 Days post administration Days post administration Days post administration Vehicle Control antibody + auristatin payload, 5 mg/kg Vehicle Cofetuzumab pelidotin, 10 mg/kg Cofetuzumab pelidotin, 5 mg/kg Control antibody + DAY301 payload Anti-DLL3 mAb + DAY301 payload, 10 mg/kg Control antibody + DAY301 payload, 10 mg/kg Control antibody + auristatin payload B7-H3 DXd ADC, 10 mg/kg Cofetuzumab antibody + DAY301 payload, 10 mg/kg Cofetuzumab pelidotin, 5 mg/kg Chemotherapy control DAY301, 5 mg/kg DAY301, 10 mg/kg Cofetuzumab mAb + DAY301 payload DAY301, 10 mg/kg * P=0.0316 Control antibody + DAY301 payload * P=0.0435 DAY301, 10 mg/kg Indicates drug administration 37 Adapted from Kong C, et al. Mol Cancer Ther. 2023;22:1128–1143. 37 3 Tumor volume (mm ) (mean ± SEM) 3 Tumor volume (mm ) (mean ± SEM) * 3 Tumor volume (mm ) (mean ± SEM) *
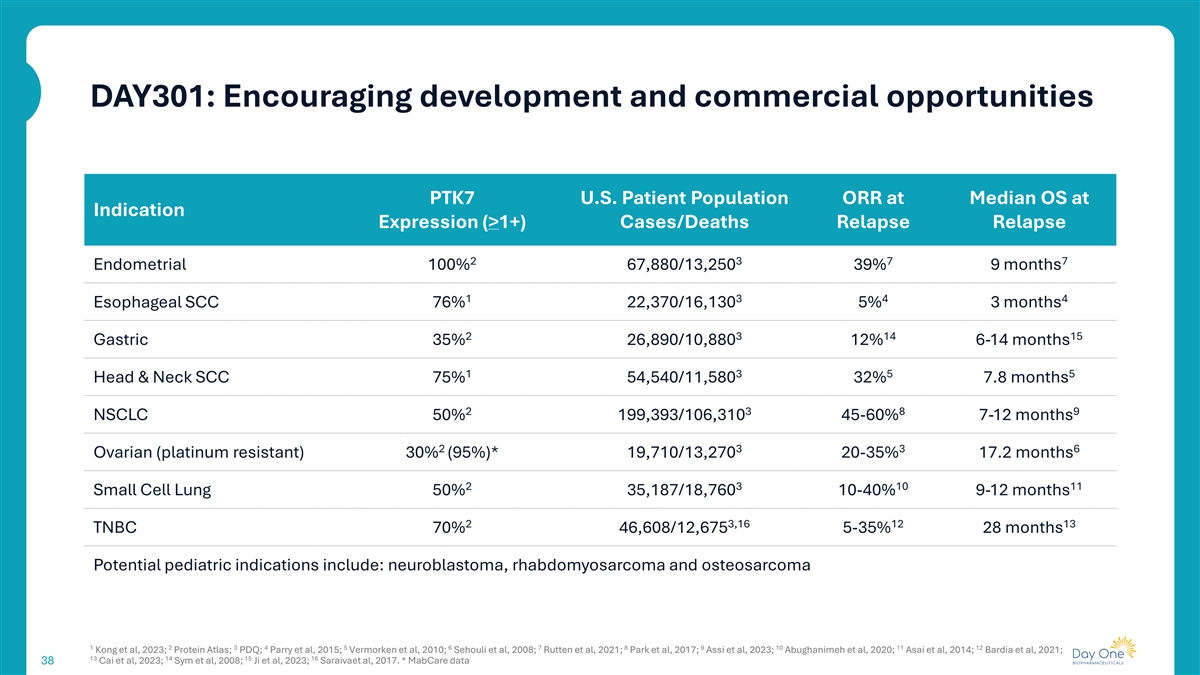
DAY301: Encouraging development and commercial opportunities PTK7 U.S. Patient Population ORR at Median OS at Indication Expression (>1+) Cases/Deaths Relapse Relapse 2 3 7 7 Endometrial 100% 67,880/13,250 39% 9 months 1 3 4 4 Esophageal SCC 76% 22,370/16,130 5% 3 months 2 3 14 15 Gastric 35% 26,890/10,880 12% 6-14 months 1 3 5 5 Head & Neck SCC 75% 54,540/11,580 32% 7.8 months 2 3 8 9 NSCLC 50% 199,393/106,310 45-60% 7-12 months 2 3 3 6 Ovarian (platinum resistant) 30% (95%)* 19,710/13,270 20-35% 17.2 months 2 3 10 11 Small Cell Lung 50% 35,187/18,760 10-40% 9-12 months 2 3,16 12 13 TNBC 70% 46,608/12,675 5-35% 28 months Potential pediatric indications include: neuroblastoma, rhabdomyosarcoma and osteosarcoma 1 2 3 4 5 6 7 8 9 10 11 12 Kong et al, 2023; Protein Atlas; PDQ; Parry et al, 2015; Vermorken et al, 2010; Sehouli et al, 2008; Rutten et al, 2021; Park et al, 2017; Assi et al, 2023; Abughanimeh et al, 2020; Asai et al, 2014; Bardia et al, 2021; 13 14 15 16 Cai et al, 2023; Sym et al, 2008; Ji et al, 2023; Saraivaet al, 2017. * MabCare data 38

DAY301: Initial Phase1a/b clinical trial design Key design elements Adult & pediatric development • BOIN design for efficiency of dose escalation • Potential adult indications include platinum resistant ovarian cancer, squamous NSCLC, esophageal SCC, HNSCC, endometrial, and/or SCLC • Backfill active dose levels to generate additional safety data • Patients to be selected based on PTK7 expression clinical trial assay • Enroll tumor types with known high PTK7 expression • Pediatric dose confirmation and efficacy assessment to begin near/at the • Advance two recommended dose levels to Phase 1b end of adult dose escalation • Final dose optimization scheme and possible registrational path(s) pending • Initial target indications include neuroblastoma, osteosarcoma, discussions with FDA at end of dose escalation/expansion rhabdomyosarcoma Phase 1b: Monotherapy Dose Expansion and Optimization Phase 1a: Monotherapy Dose Escalation DL5 Go to dose Expand to a potential single-arm RD1 cohort RD1 optimization registrational trial for accelerated Simon 2-stage approval or randomized trial at DL4 design optimized dose RD2 cohort DL3 RD1 RD2 Phase 1: Pediatric DL2 Identify two recommended RD2 Monotherapy Dose Lower of the two dose levels for further RD1 adult RDs Confirmation DL1 evaluation, based on safety and anti-tumor activity FDA-cleared RD-1 starting dose DL, Dose Level; RD, Recommended Dose; BOIN, Bayesian Optimal Interval; HNSCC, Head and Neck Squamous Cell Carcinoma; SCLC, Small Cell Lung Cancer; SCC, Squamous-Cell Carcinoma; NSCLC, Non-Small Cell 39 Lung Cancer

Summary 40
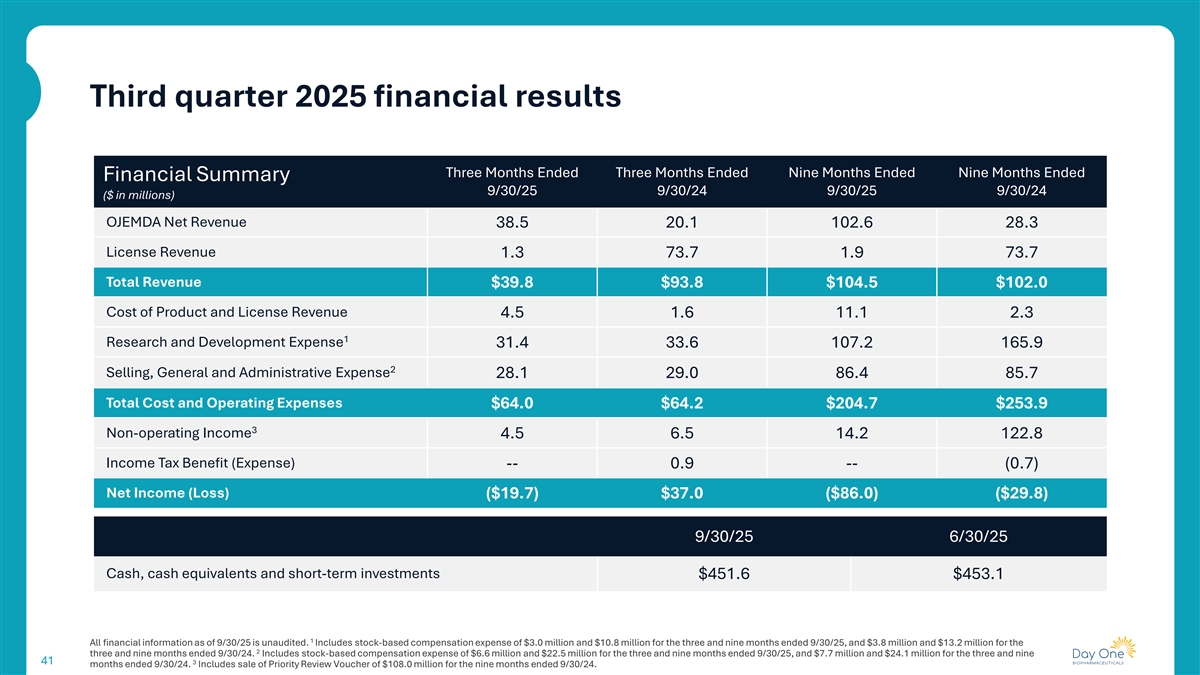
Third quarter 2025 financial results Three Months Ended Three Months Ended Nine Months Ended Nine Months Ended Financial Summary 9/30/25 9/30/24 9/30/25 9/30/24 ($ in millions) OJEMDA Net Revenue 38.5 20.1 102.6 28.3 License Revenue 1.3 73.7 1.9 73.7 Total Revenue $39.8 $93.8 $104.5 $102.0 Cost of Product and License Revenue 4.5 1.6 11.1 2.3 1 Research and Development Expense 31.4 33.6 107.2 165.9 2 Selling, General and Administrative Expense 28.1 29.0 86.4 85.7 Total Cost and Operating Expenses $64.0 $64.2 $204.7 $253.9 3 Non-operating Income 4.5 6.5 14.2 122.8 Income Tax Benefit (Expense) -- 0.9 -- (0.7) Net Income (Loss) ($19.7) $37.0 ($86.0) ($29.8) 9/30/25 6/30/25 Cash, cash equivalents and short-term investments $451.6 $453.1 1 All financial information as of 9/30/25 is unaudited. Includes stock-based compensation expense of $3.0 million and $10.8 million for the three and nine months ended 9/30/25, and $3.8 million and $13.2 million for the 2 three and nine months ended 9/30/24. Includes stock-based compensation expense of $6.6 million and $22.5 million for the three and nine months ended 9/30/25, and $7.7 million and $24.1 million for the three and nine 41 3 months ended 9/30/24. Includes sale of Priority Review Voucher of $108.0 million for the nine months ended 9/30/24.

Day One is well positioned for sustainable growth and long-term success Execute on clinical Drive OJEMDA development pipeline for revenue growth FIREFLY-2 and DAY301 Leverage our development and Maintain strong capital commercialization expertise to position while investing in further expand our multiple our pipeline asset portfolio 42 42

Appendix 43
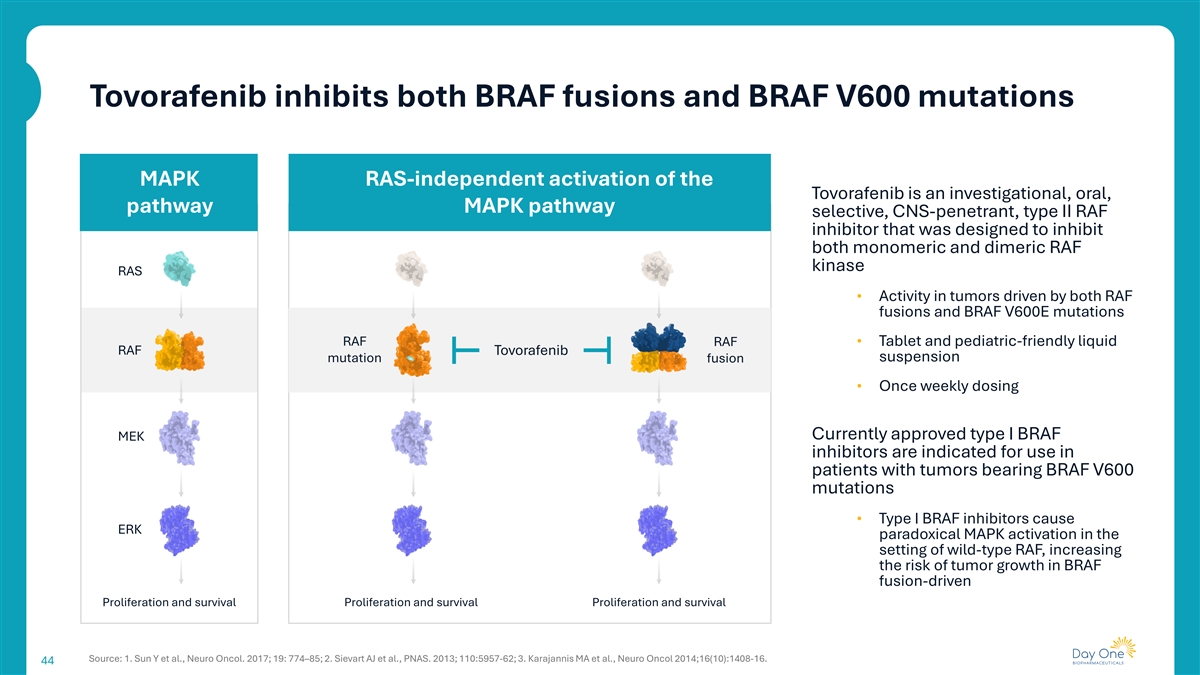
Tovorafenib inhibits both BRAF fusions and BRAF V600 mutations MAPK RAS-independent activation of the Tovorafenib is an investigational, oral, pathway MAPK pathway selective, CNS-penetrant, type II RAF inhibitor that was designed to inhibit both monomeric and dimeric RAF kinase RAS • Activity in tumors driven by both RAF fusions and BRAF V600E mutations RAF RAF • Tablet and pediatric-friendly liquid RAF Tovorafenib suspension mutation fusion • Once weekly dosing Currently approved type I BRAF MEK inhibitors are indicated for use in patients with tumors bearing BRAF V600 mutations • Type I BRAF inhibitors cause ERK paradoxical MAPK activation in the setting of wild-type RAF, increasing the risk of tumor growth in BRAF fusion-driven Proliferation and survival Proliferation and survival Proliferation and survival Source: 1. Sun Y et al., Neuro Oncol. 2017; 19: 774–85; 2. Sievart AJ et al., PNAS. 2013; 110:5957-62; 3. Karajannis MA et al., Neuro Oncol 2014;16(10):1408-16. 44